An 'Ascite-ing' Case of Abdominal Distention
Overview of Treatment Options in Budd Chiari Syndrome
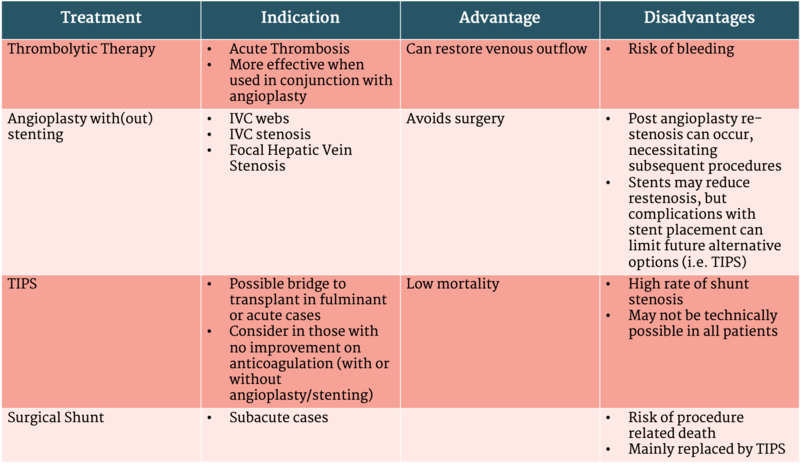
The recommended treatment strategy for Budd Chiari Syndrome consists of a step wise approach (see Figure 1, Table 1).
Figure 1: Stepwise Approach to Management of Budd-Chiari Syndrome
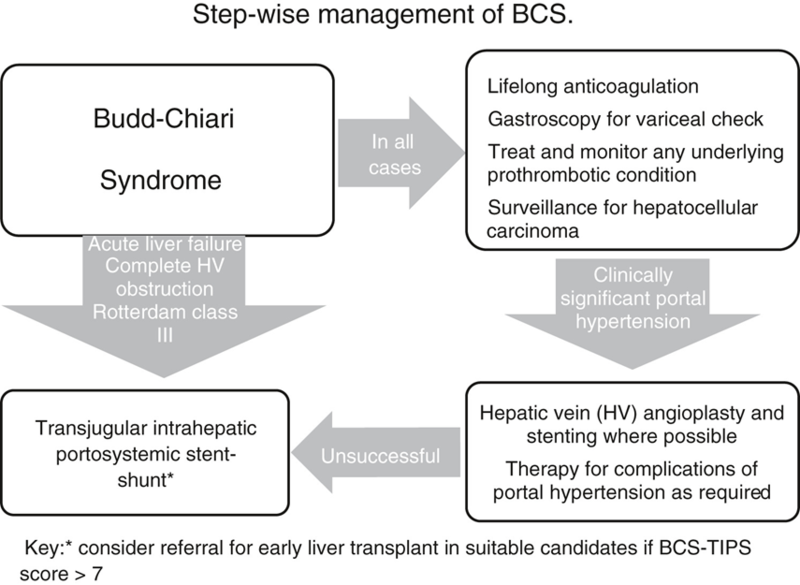
Taken from: Khan, F., et al., Review article: a multidisciplinary approach to the diagnosis and management of Budd-Chiari syndrome. Aliment Pharmacol Ther, 2019. 49(7): p. 840-863
1. Treat predisposing conditions and prevent propagation of the clot with anticoagulation:
- An underlying risk factor for thrombosis (inherited or acquired thrombophilia, systemic or hormonal factors) is present in 79-84% of cases.
- Referral to a hematologist is recommended for initiation of targeted therapies such as cytoreductive and anti-complement agents in myeloproliferative disorders and paroxysmal nocturnal hemoglobinuria, respectively.
- AASLD guidelines recommend maintaining long term anticoagulation therapy unless a major contra-indication is present or complications of anticoagulation occur.
- Low molecular weight heparin can be used in the acute setting and vitamin K antagonists for long term treatment
- Direct acting oral anticoagulants (DOACs) have been used in case reports, but are not FDA approved for this indication; if used, must be done with caution, particularly in patients with renal failure.
2. Restore patency of thrombosed vein
- Angioplasty can potentially restore hepatic outflow, particularly in patients with partial or segmental stenosis. Therefore, once a diagnosis of BCS is made, patients with short length venous stenosis amenable to angioplasty/stenting should be quickly identified and referred to interventional radiology
- Thrombolytic therapy is an option for an acute clot, but evidence for these agents is limited to small case series and individual reports.
- Can be more effective in re-establishing patency of the vessel when used in conjunction with angioplasty.
3. Creation of shunts can decompress the liver by creating an alternative venous outflow tract
- No data to suggest when referral for TIPS should be placed. AASLD recommends insertion of TIPS should be considered in patients without improvement on anticoagulation therapy and in those who are unresponsive to or who may not be candidates for angioplasty/stenting.
- In those with complete hepatic vein obstruction, TIPS may not be technically feasible and direct intrahepatic portosystemic shunt (DIPS) can be considered.
- Several variations of surgical shunts have been used depending on technical limitations of the case.
- High perioperative mortality and shunt dysfunction are important considerations to this option.
- Surgical shunts have been replaced by less invasive TIPS
4. Liver transplantation should be considered if:
- TIPS insertion fails or does not improve clinical condition or
- Fulminant hepatic failure