To Band or Not To Band? Esophageal Varices in the Pediatric Population
Quick recap of anatomy:
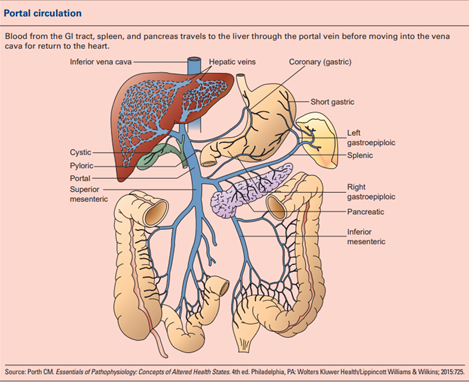
Approximately, 2/3rd of blood supply to the liver is via the portal vein. Increase in amount of blood flow, resistance, or both will increase portal pressures. The changes in blood flow can be either in the relatively large vessels like main portal vein or in the sinusoidal circulation within the liver. This causes elevated vascular resistance and portal hypertension. As a response to the elevated pressure in the system, splanchnic vasodilation occurs, which increases portal flow, worsening the portal pressures.
Defining Portal Hypertension
Normal portal venous system pressures are between 5-10 mmHg. Hepatic venous pressure gradients (HVPG) are typically used as a surrogate for portal pressures. HVPG is the difference between a free hepatic vein pressure (FHVP) and a wedged hepatic vein pressure (WHVP). Normal values are typically 1-4mmHg. Portal hypertension is characterized by a HVPG >5mmHg. In adults, HVPG measurements above 10mmHg are associated with the development of esophageal varices and measurements >12mmHg are associated with complications such as ascites and variceal bleeding
HVPG measurements can be helpful in certain clinical scenarios in children. Elevated HVPG can be seen in sinusoidal and post sinusoidal causes of portal hypertension, like cirrhotic or cholestatic liver diseases. In a single center study children with portal hypertension, about 18% had a prehepatic cause for portal hypertension, in whom HVPG is often normal and less informative. Another retrospective study found that HVPG measurements in children do not correlate with varices, risk of variceal bleeding or hepatic fibrosis. Although feasible and safe, HVPG is seldom used in pediatric population in practice due its invasive nature and somewhat limited clinical application.
An operational definition of portal hypertension in children, based on clinical symptoms, is frequently used in the research and clinical setting. This defines clinical evident portal hypertension (CEPH) as follows.
Definite CEPH (dCEPH): One or both of:
- Clinical Findings, which consists of both:
- Splenomegaly (spleen size > 2 cm below the costal margin by physical examination) and
- Platelet count < 150 × 109/L (= 150,000/mm3= 150,000/micro-L = 150,000/µL = 150,000/mcL)
- Manifestations, which consist of at least one of:
- Clinically evident ascites or
- Endoscopic evidence of esophageal or gastric varices
Possible CEPH (pCEPH): Absence of manifestations listed above and only one of:
- Splenomegaly (spleen size > 2 cm below the costal margin by physical examination) or
- Platelet count < 150 × 109/L (= 150,000/mm3= 150,000/micro-L = 150,000/µL = 150,000/mcL)
Absent CEPH (aCEPH): Absence of any of the above manifestations or findings
Causes of Portal Hypertension
The table below summarizes many of the causes of portal hypertension in the pediatric population. Biliary atresia and extrahepatic portal vein obstruction (EHPVO) are the most common causes of portal hypertension in children. While EHPVO is more common in the developing countries, biliary atresia is a common cause in the developed countries, especially in the USA.
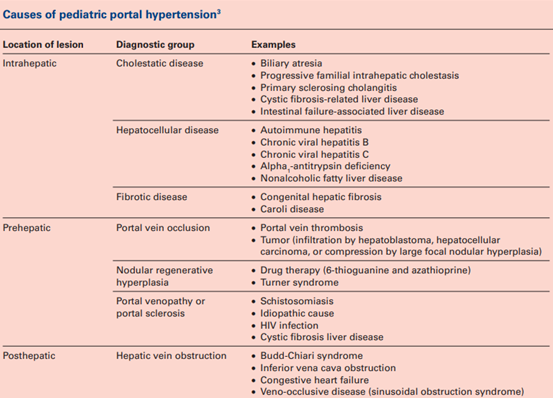
Procoagulant and proinflammatory states are risk factors for EHPVO. Specifically in children, omphalitis, umbilical vein cannulation, abdominal infections/sepsis, surgeries or trauma can increase the risk of EHPVO.
Variceal Bleeding in Pediatric Patients
Early identification of high-risk varices and their treatment is the cornerstone management of portal hypertension. AASLD practice guidelines recommend a screening endoscopy in adult patients with portal hypertension and follow up of high-risk varices every 2-3 years . Treatment of medium to large sized varices is recommended. However, in children, the Baveno meeting consensus was not conclusive about the utility of surveillance EGDs and primary prophylaxis of varices in children. The suggestions were to consider EGD based on clinical criteria such as splenomegaly, thrombocytopenia (<100,000), with an intention to treat on a case-to-case basis.
The incidence of a variceal bleed in children is relatively low compared to adults. Esophageal varices have been reported in about 70% of children with biliary atresia, or portal vein thrombosis. Incidence of variceal bleeding is about 6-20% in children, depending on the etiology of liver disease. Recurrent variceal bleeding or rebleeding from varices occurs in about 7% of children with varices. In a recent study done through the ChiLDReN network, over a period of 16 years, the incidence of variceal hemorrhage in children with BA, who survived with their native livers was about 8-9%. Mortality from variceal bleeding is lower in children than adults. Endoscopy is an invasive procedure, requiring anesthesia; given these factors as well as a lower incidence of variceal bleeding in children, primary prophylaxis for varices in children varies by practice. Endoscopy can be used to identify and characterize varices and hence support the diagnosis of dCEPH in cases where clinical findings alone are not sufficient to make the diagnosis.
Noninvasive Screening for Varices
Radiological tools such as ultrasound can be useful adjuncts in children with portal hypertension to assess the anatomy, presence of ascites as well as reversal of flow in the portal vein (although this is a late finding). In adults, use of US based techniques like spleen and liver stiffness, portal vein velocities and portal vein dimensions are being studied as tools to predict clinically significant portal hypertension . Liver stiffness measures along with low platelets is a predictor for high grade varices in adults. Single center studies have shown that spleen stiffness measurements in children could be used to predict varices; however, larger validation studies are needed.
Blood based biomarkers and scoring systems which include makers of endothelial dysfunction, metabolic dysfunction and fibrosis makers are being studied as predictor for portal hypertension and variceal bleeding in adults. Biomarkers which can predict portal hypertension and varices based on markers for endothelial dysfunction look most promising in children, since they can identify both pre hepatic and hepatic causes for PH.
Management of Variceal Hemorrhage
Acute hemorrhage from variceal bleed is a medical emergency in children. The blood loss is often significant causing hemodynamic compromise. Variceal hemorrhage requires stabilization via volume resuscitation, often with crystalloid or blood product administration (usually to a hemoglobin goal of 7-9 g/dl). Other considerations based on the severity and presentation of the patient are octreotide, IV antibiotics and IV PPI as other reasons for bleeding such as portal hypertensive gastropathy and/or gastric ulcerations may be present. Upper endoscopy is the next step in therapy once the patient is hemodynamically stable.
Varices with a high risk of bleeding such as size > grade 2 or features of recent bleeding such as the red wale sign should be treated endoscopically. Band ligation or sclerotherapy may be performed. Band ligation is preferred over sclerotherapy due to more efficient eradication results in adults. However, in infants and smaller children (<10 kg), sclerotherapy may be preferred if the banding apparatus is too large to pass the upper esophageal sphincter.
Medical Management of Varices
Beta blockers are approved for use in adults with CSPH and clinically significant varices, as a primary prophylaxis to prevent VH. Non-selective beta blockers reduce the cardiac output through β1 blockage and cause splanchnic vasoconstriction via β2 blockage. Reduction in heart rate and blunting of vagal responses are concerning side effects in children. Currently, due to lack prospective randomized trials in children, they are not recommended for use and clinical practice on beta blockers in pediatric variceal bleeding is variable. The combination of NSBB and secondary endoscopic prophylaxis did not show any significant benefit in children.
Surgical Management of Varices
For refractory symptoms of portal hypertension (ascites, UGI bleeding) not controlled by medication or endoscopic means, interventional radiology or surgical intervention can be considered. Occasionally portal vein venoplasty with or without stent placement, performed by interventional radiology, is utilized to avoid shunt surgery.
The choice of shunt surgeries depends on liver architecture, etiology of portal hypertension and vascular anatomy and include Meso Rex bypass shunt, distal splenorenal shunts, or transjugular intrahepatic portosystemic shunts. Meso Rex shunt is the shunt surgery of choice for children with extrahepatic portal venous obstruction by reestablishing first pass portal perfusion, though a prerequisite for the shunt is preserved liver architecture. In patients with refractory symptoms of portal hypertension, liver transplantation may be indicated.

