Just Another Case of Hepatic Encephalopathy?

Epidemiology of Intracranial hemorrhage in cirrhosis patients
Multiple studies have examined the epidemiology of intracranial hemorrhage (ICH) and compared the incidence of ICH in patients with cirrhosis and without cirrhosis. In a retrospective study of over 1.5 million Medicare patients, of whom 15,586 had cirrhosis, patients with cirrhosis had a higher incidence of ICH, with a hazard ratio of 1.9 compared to those without cirrhosis; ICH was more common in cirrhosis patients than ischemic stroke. The annual incidence of ICH in cirrhosis patients in this study was 0.31%. A meta-analysis of slightly over 93,000 patients showed a pooled incidence of 2.0% for ICH in cirrhosis patients. Furthermore, cirrhosis was shown to be a risk factor for ICH in this meta-analysis, while it was not for ischemic strokes.
Figure 1 - Comparison of ICH and ischemic strokes in patients with and without cirrhosis
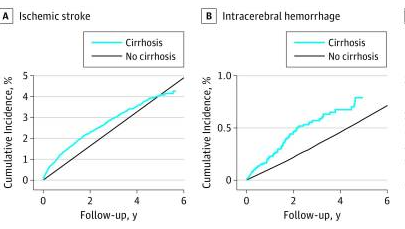
Taken from: Association Between Cirrhosis and Stroke in a Nationally Representative Cohort. JAMA Neurol 2017.
Who to Assess for ICH and Outcomes
Due to the high prevalence of hepatic encephalopathy (HE) in patients with cirrhosis, and the lack of clinical utility of head CT in cirrhosis patients who present with HE and altered mental status, the question of which patients with cirrhosis and altered mental status to obtain head CTs in is pertinent. One retrospective cohort study attempted to answer this clinical quandary. The study examined 462 cirrhosis patients over ten years who were admitted to the hospital with altered mental status and received a head CT. Approximately 3% were diagnosed with ICH; risk factors for ICH were falls, trauma, history of ICH, and focal neurologic findings. Thrombocytopenia and elevated INR were not associated with ICH. The number needed to scan to diagnose ICH was nine for focal neurologic deficits, twenty for falls and trauma, and 293 for altered mental status without focal deficits or trauma.
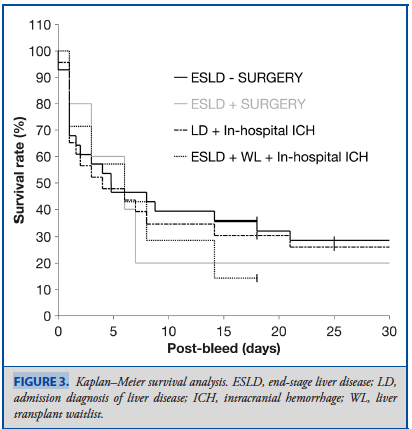
Survival outcomes for cirrhosis patients with ICH are poor. A retrospective review from 53 patients with liver disease who developed ICH showed an overall survival of 22%. Survival for those patients on the liver transplant waitlist was 14%, with only one patient surviving. Patients who underwent surgical evacuation of the hematoma did not have a significant survival benefit compared to those who were managed non-operatively.
Figure 2 - Survival after ICH in four different groups
Management of Intracranial Hemorrhage in Patients with Cirrhosis
Management of intracranial hemorrhage in cirrhosis is challenging due to patient complexity and poor surgical outcomes. Treatment often encompasses multidisciplinary care involving neurosurgery, hepatology, and neurocritical care teams. The role of hepatology in this care is often to manage cirrhosis-related complications, however hepatology should also be involved in discussions surrounding INR, fibrinogen, and platelet goals. The management of patients with cirrhosis and ICH who have elevated INR, low fibrinogen, and low platelets is complex and nuanced.
In patients without cirrhosis who experience ICH and are on warfarin, elevated INR is clearly predictive of increased bleeding risk. In this population, The American Society of Hematology recommends warfarin reversal with 4-factor PCC until INR normalizes. However, in cirrhosis, we know that INR alone is a poor predictor of bleeding risk. Furthermore, transfusion of large volumes of blood products, including fresh frozen plasma (FFP), can increase portal pressures and increase risk of variceal bleeding. Therefore, a judicious and thoughtful approach to transfusion of blood products is warranted.
Consideration of measuring coagulopathy by a more dynamic measure, like thromboelastography (TEG) or rotational thromboleastography (ROTEM) may be warranted. One RCT demonstrated that TEG was helpful in decreasing prophylactic blood product transfusions in patients with cirrhosis, without any change in bleeding risk, peri-procedurally. However, currently, there are no good studies/data to guide the use of TEG/ROTEM in intracranial hemorrhage in cirrhosis.
Low platelets in cirrhosis may be related to bleeding risk, platelets goals are often > 100,000 for central nervous system bleeding. Fibrinogen goals are generally > 100-120 in central nervous system bleeding, with preferable use of cryoprecipitate which is associated with a smaller volume load than FFP. However, these goals are not based on great data, as there is mixed data on whether transfusing platelets or fibrinogen improves outcomes.
Taken from: Survival Outcomes after Intracranial Hemorrhage in Liver Disease. Op Neuro 2019.
