A puzzling case of portal hypertension: a collision between hema- and hepatology
A primer on portal hypertension
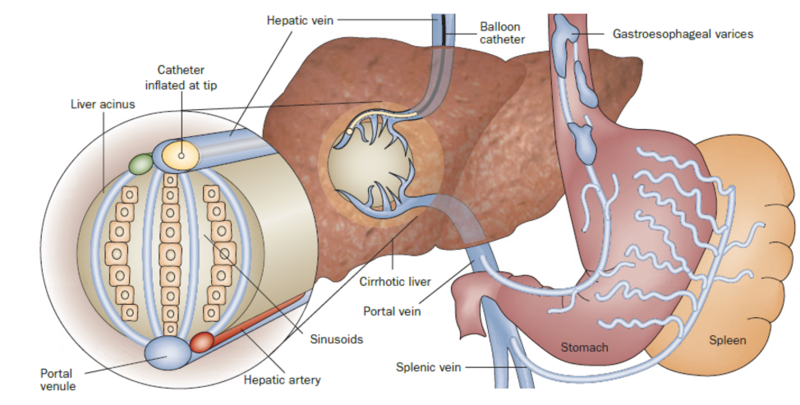
Portal hypertension is the result of resistance to portal blood flow and is defined as an HVPG above 5 mmHg. The HVPG represents the pressure differential between the portal vein and inferior vena cava. This can be calculated by subtracting the free hepatic vein pressure (reflects intra-abdominal pressure) from the wedged hepatic vein pressure (represents hepatic sinusoidal pressure as an estimation of portal pressure) as shown in Figure 1.
Figure 1 - Measurement of portal pressures
Taken from: The clinical use of HVPG measurements in chronic liver disease. Nat Rev Gastroenterol Hepatol Oct 2009
Clinically significant sequelae, such as variceal formation, develop at an HVPG ≥ 10 mmHg and an HVPG ≥16 mm Hg portends elevated risk for decompensation events (variceal hemorrhage, ascites, hepatic encephalopathy). Portal hypertension is generally classified into three categories: prehepatic, intrahepatic, and posthepatic as shown in Figure 2.
Figure 2: Classification and common causes of portal hypertension
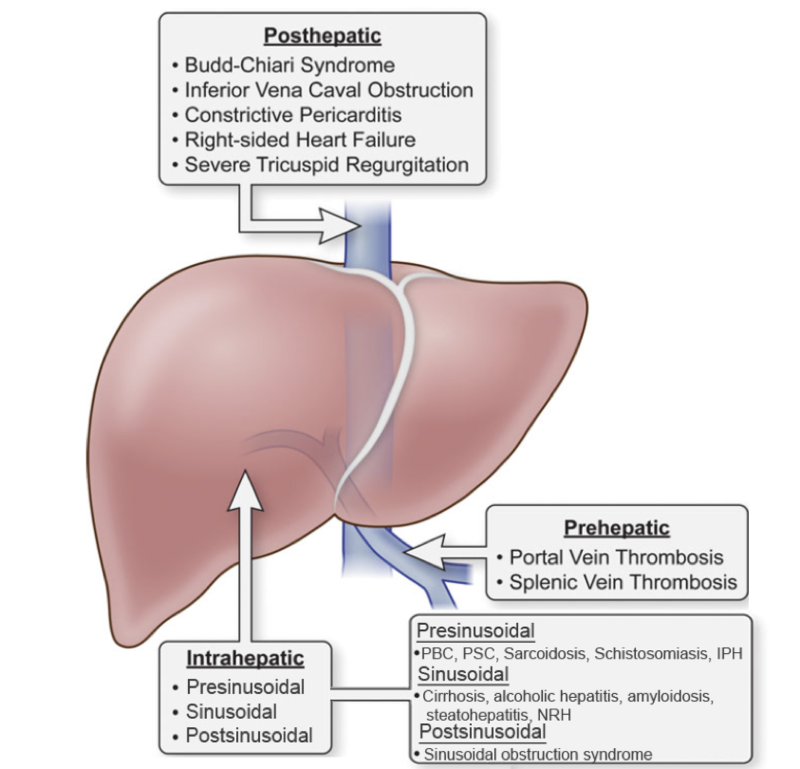
Image modified from: Koh C, Heller T. Approach to the diagnosis of portal hypertension. Clinical Liver Disease. 2012.
What is noncirrhotic portal hypertension?
As the name suggests, NCPH encompasses many conditions that cause portal hypertension in the absence of underlying cirrhosis.
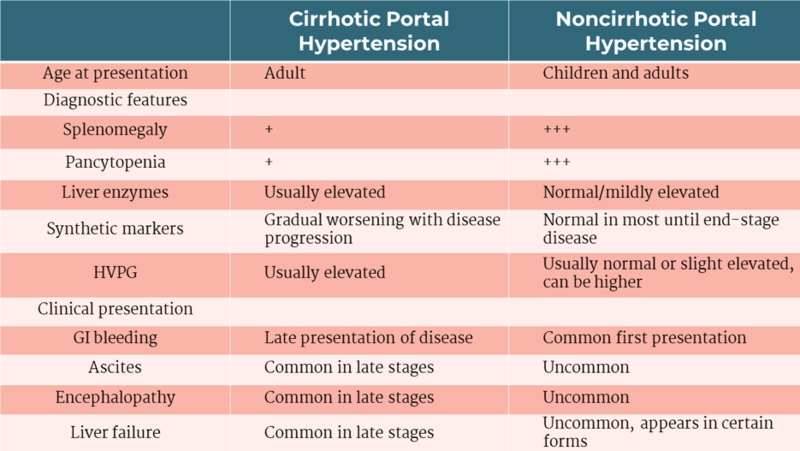
Table 1 shows key differences in clinical presentation and laboratory markers of portal hypertension in patients with cirrhosis compared to patients with NCPH.
Table 1: Presentations of cirrhotic and noncirrhotic portal hypertension.
Adapted from: Etzion O, Koh C, Heller T. Noncirrhotic portal hypertension: An overview. Clinical Liver Disease. 2015.
Evaluation
NCPH is often underrecognized. Prompt recognition of this condition is essential as it can lead to significant complications and chronic liver disease. However, diagnosis can be challenging due to lack of reliable noninvasive tests. Laboratory and imaging findings can vary, and even histopathological examination may miss rare causes as additional stains may not be readily available.
Gradually decreasing platelet count and hypersplenism should prompt evaluation for portal hypertension, particularly in patients with disorders associated with NCPH. This should include an evaluation for common causes of chronic liver disease such as alcoholic liver disease, nonalcoholic steatohepatitis, chronic viral hepatitis B and C, autoimmune hepatitis, primary biliary cholangitis, iron overload conditions like hereditary hemochromatosis, alpha-1 antitrypsin deficiency, and Wilson disease. Doppler ultrasonography can be helpful to rule out extrahepatic causes. An echocardiogram to rule out right-sided heart failure should also be obtained. Liver biopsy and pressure measurements should be pursued and reticulin staining should be performed.
While an elevated HVPG can be helpful, it is important to note that this measurement may be normal or only minimally elevated in patients with NCPH. Furthermore, there is no meaningful correlation between an elevated HVPG and the development of ascites or variceal bleeding in this patient population. Common causes of NCPH are presinusoidal or prehepatic and therefore may not cause an elevated wedged pressure. Additionally, the portal system pressure may be underestimated in cases of intrahepatic shunting. Therefore, even if HVPG is normal, individually elevated wedged hepatic vein pressure and/or elevated free hepatic vein pressure should be noted.
Idiopathic portal hypertension is a possibility when all other etiologies of portal hypertension have been excluded.
What is NRH?
Nodular regenerative hyperplasia is a benign condition in which the hepatic parenchyma is transformed into small, regenerative nodules in the absence of fibrosis. NRH causes NCPH and is often grouped with other distinct histopathologic features to form the clinical entities “idiopathic portal hypertension,” “idiopathic noncirrhotic portal hypertension,” “hepatoportal sclerosis,” or “noncirrhotic portal fibrosis.” We will focus on NRH alone. Similar to other causes of NCPH, NRH can commonly present with variceal bleeding, and ascites.
Diagnosis of NRH
Diagnosis is based on histology; reticulin staining can demonstrate micronodules comprised of highly proliferative hepatocytes surrounded by a compressed reticulin network and internodular areas of hepatocyte atrophy without fibrosis. Although biopsy is the gold standard for diagnosis, interobserver agreement has been reported as low and is subject to sampling error. The use of magnetic resonance elastography to aid in the diagnosis of NRH has also been studied. While the data looks promising, further studies are necessary prior to implementing the use of MRE as a diagnostic tool for NRH.
Associations with NRH
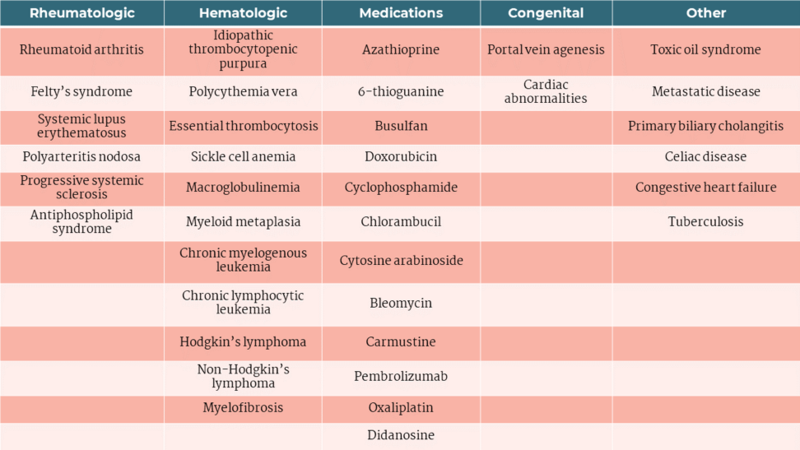
NRH has been associated with multiple conditions, including rheumatologic, dermatologic, and hematologic disorders and solid organ and bone marrow transplant. Medications such as chemotherapeutic agents and azathioprine used in inflammatory bowel disease or as part of an immunosuppressive regimen after liver transplantation are also linked with the development of NRH. More recently, NRH was also associated with immune checkpoint inhibitors which are used to treat various malignancies. Table 2 provides a list of associations with NRH.
Table 2: Disorders and medications associated with NRH
Adapted from: Reshamwala PA, Kleiner DE, Heller T. Nodular regenerative hyperplasia: Not all nodules are created equal. Hepatology. 2006.
Treatment of NRH
Treatment is aimed at removing or addressing the cause. Portal hypertension is managed with diuretics for ascites, endoscopic variceal ligation of varices, and non-selective beta blockade in certain cases. Treatment of severe portal hypertension includes surgical shunts or transjugular intrahepatic portosystemic shunt (TIPS) placement. As NRH is rare, large studies are not available. TIPS may be a reasonable option in patients with NRH and complications from portal hypertension. In a multicenter retrospective study, 41 patients underwent TIPS either for bleeding varices (61%) or refractory ascites (39%). Survival was 80% at 2- years and worse outcomes were noted in patients with renal dysfunction and extrahepatic comorbidities.
Occasionally, patients will develop progressive liver failure or refractory portal hypertension requiring transplantation. Manzia et al conducted a systematic review of the role of transplantation in NRH and found 11 studies in which 26 patients were transplanted for NRH. These patients had significant sequalae of portal hypertension. The 5-year patient survival rate was 78.3% with a mortality rate of 19.2%. One patient developed recurrent NRH post-transplant. The authors concluded that liver transplantation was a viable treatment strategy for patients with NRH. Meijer et al examined explanted livers and found NRH in 11 of 1886 patients who underwent liver transplantation over a 20-year period in the Netherlands. The 1-year and 5-year survival rate was 82% and 73%, respectively. NRH recurrence was noted in one patient 14 years after transplantation. Larger studies with longer follow up are necessary.