Steatotic-What? Changes in Fatty Liver Nomenclature
MASLD
Metabolic dysfunction-associated steatotic liver disease (MASLD) refers to the presence of hepatic steatosis when no other causes for secondary hepatic fat accumulation are present, and patients have one or more cardiometabolic risk factors. Patients with MASLD may have steatosis with or without inflammation and fibrosis.
Metabolic associated steatohepatitis (MASH) is a subdivision of MASLD in which inflammation and cellular injury are present, usually evidenced by an elevation in aminotransferases. The hepatic inflammation may be histologically indistinguishable from alcohol-associated steatohepatitis.
Prevalence
MASLD is a highly prevalent cause of chronic liver disease. In the United States, studies report a prevalence of 10 – 46 percent, while worldwide MASLD has a reported prevalence of 6 to 35 percent. MASLD has also been rising in pediatric populations, with a current prevalence of 5-10%.
Clinical manifestations:
Most patients with MASLD are asymptomatic. Patients often present with incidental labs revealing elevated liver aminotransferases and/or hepatic steatosis on abdominal imaging. Mild to moderate elevations in AST/ALT (two to five times the upper limit of normal) are typical, although normal levels do not exclude MASLD. Alkaline phosphatase may also be elevated (two to three times the upper limit of normal). Serum albumin and bilirubin levels are typically within normal range until patients develop advanced fibrosis/cirrhosis. Patients with MASLD may also have an elevated ferritin concentration or transferrin saturation. A serum ferritin greater than 1.5 times the upper limit of normal in patients with MASLD is associated with a more hepatic fibrosis.
Differential Diagnosis
Alternate causes of hepatic steatosis
- Alcohol-associated liver disease
- Hepatitis C (particularly genotype 3)
- Wilson disease
- Starvation
- Medications
- Drug-Induced liver injury
- Acute fatty liver of pregnancy
- Reye Syndrome
- Inborn errors of metabolism
- Lipodystrophy
New Nomenclature
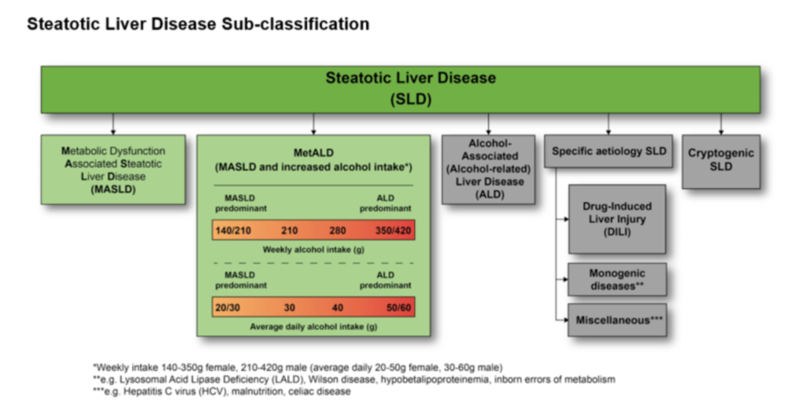
Figure from Rinella et al: A multi-society Delphi consensus statement on new fatty liver disease nomenclature.
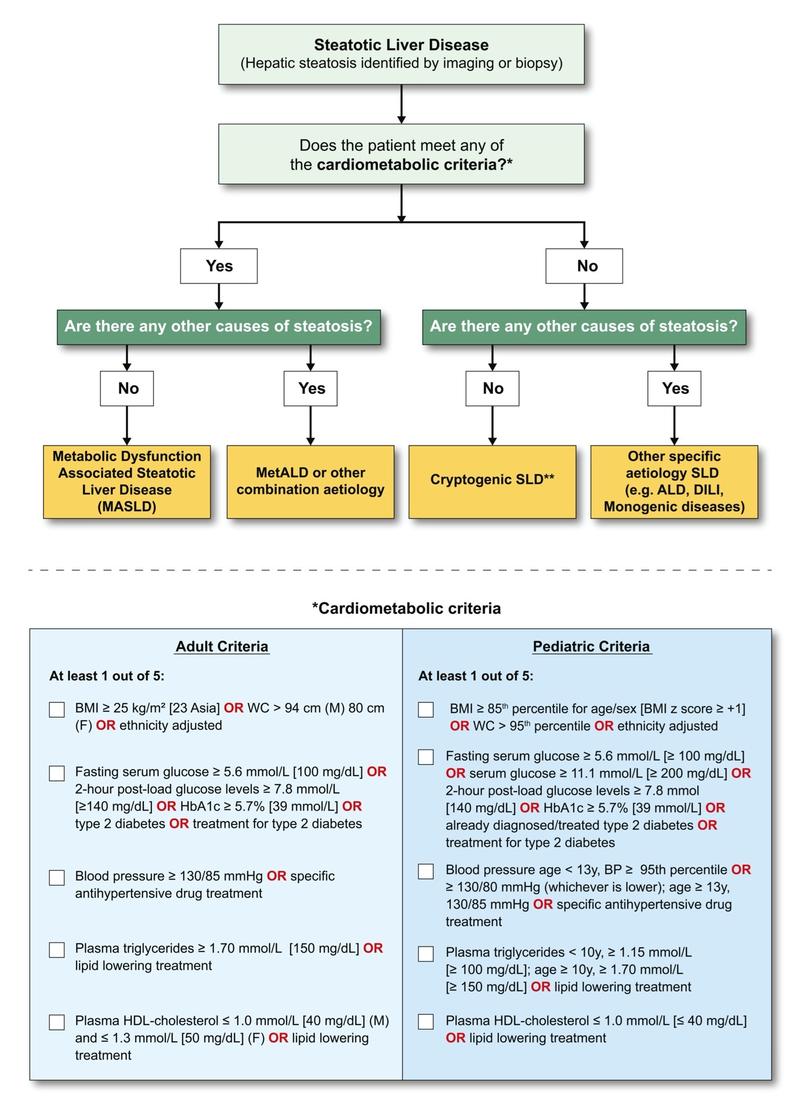
In June 2023, a new nomenclature for the spectrum of NAFLD was adopted. Several factors were considered in this change. The prior terminology included stigmatizing language around patients with alcohol use disorder and obesity (“nonalcoholic” and “fatty”) and did not accurately describe underlying risk factors or pathophysiology. There was a need for new terminology that reflected the role of metabolic dysfunction in the development of what is now termed MASLD. Furthermore, there was a need for a disease classification that incorporated both alcohol and metabolic disease because the overlap is quite common.
- Steatotic Liver Disease is now the term that encompasses the various etiologies of steatosis (diagnosed histologically or by imaging).
- Non-alcoholic fatty liver disease (NAFLD) was changed to metabolic dysfunction-associated steatotic liver disease (MASLD). MASLD is defined by the presence of hepatic steatosis with at least one of five cardiometabolic risk factors (BMI > 25, Prediabetes/Diabetes, Hypertension, Hyperlipidemia, Low HDL)
- MetALD (MASLD and increased alcohol intake) is the new term for patients with MASLD who consume high amounts of alcohol per week, (140 g/week in females and 210g/week in males)
- NASH was replaced with Metabolic dysfunction-associated steatohepatitis (MASH).
- Patients with no metabolic risk factors or other identifiable cause of steatosis are now categorized as cryptogenic steatotic liver disease.
Diagnosis and Diagnostic Modalities
Diagnosis usually begins with a thorough history to identify potential causes of liver disease such as significant alcohol use, rapid weight loss, and an assessment of all medications and supplements. All patients should be tested for chronic viral hepatitis (hepatitis B and C). Immunity to hepatitis A and B should also be assessed to determine if vaccinations are required. Other chronic liver diseases such as autoimmune hepatitis, hemochromatosis, alpha-1 antitrypsin, and Wilson disease should be considered and further testing should be pursued if indicated.
In patients who have not undergone abdominal imaging, an ultrasound should be obtained. Ultrasound has good sensitivity and specificity for hepatic steatosis in the general population, however the sensitivity is decreased in patients who are obese. Vibration controlled transient elastography (VCTE, or Fibroscan© ) can be used to evaluate extent of fibrosis and a controlled attenuation parameter (CAP) score to evaluate the extent of hepatic steatosis. Both CT and standard-protocol MRI can identify steatosis, but neither are sufficiently sensitive to detect inflammation or fibrosis. Magnetic resonance spectroscopy allows for quantification of hepatic fat but is not widely available.
Although liver biopsy is the gold standard for diagnosing MASLD/MASH, most cases can be diagnosed with history, laboratory tests, and imaging findings. In patients who continue to have an unclear diagnosis following a noninvasive evaluation, a liver biopsy should be considered.
Figure from Rinella et al: A multi-society Delphi consensus statement on new fatty liver disease nomenclature.
Identifying risk of advanced liver fibrosis or cirrhosis
One challenge in clinical practice is the identification of those with advanced liver fibrosis or cirrhosis. Although liver biopsy helps determine the stage of liver fibrosis in MASLD, it is not the most accessible or realistic option in most settings.
Non-invasive tests for liver fibrosis are widely available, and an area of ongoing research. A more detailed post on the non-invasive assessment of fibrosis in MASLD will be available soon in the Clinical Pearls series. Approaches to non-invasive screening include lab-based screening such as the Fibrosis-4 score (FIB-4), and secondary risk assessment by vibration-controlled elastrography (VCTE), magnetic resonance elastography (MRE), or the Enhanced Liver Fibrosis test (ELF). A FIB-4 score of ≥ 1.3 may indicate the presence of fibrosis and warrants further evaluation with a secondary fibrosis assessment method (VCTE, MRE, ELF). However, non-invasive evaluation of fibrosis in MASLD is not perfect and may not perform as well in patients with significant obesity. As such, liver biopsy should be strongly considered when clinicians are not highly confident in the results of non-invasive tests.
Take home points
- MASLD refers to the presence of hepatic steatosis when no other causes for secondary hepatic fat accumulation are present, and patients have one or more cardiometabolic risk factors
- Fatty liver disease terminology has changed as of June 2023. MASLD has replaced NAFLD and MASH has replaced NASH.
- Steatotic Liver Disease refers to the spectrum of diseases that cause hepatic steatosis.
- MetALD refers to patients with MASLD who consume high amounts of alcohol per week, (140 g/week in females and 210g/week in males)
- Patients with MASLD or MetALD should receive non-invasive testing of fibrosis.
- FIB-4 is readily available to non-GI/hepatology providers and is a good initial screening test for fibrosis, particularly where VCTE is not available.
- In patients with FIB-4 >= 1.3, a secondary assessment should be performed, preferably with VCTE or MRE to evaluate for advanced fibrosis.