The Cardiology-Hepatology Axis-Fontan Associated Liver Disease
But what is Fontan Physiology and how does it impact the Liver?
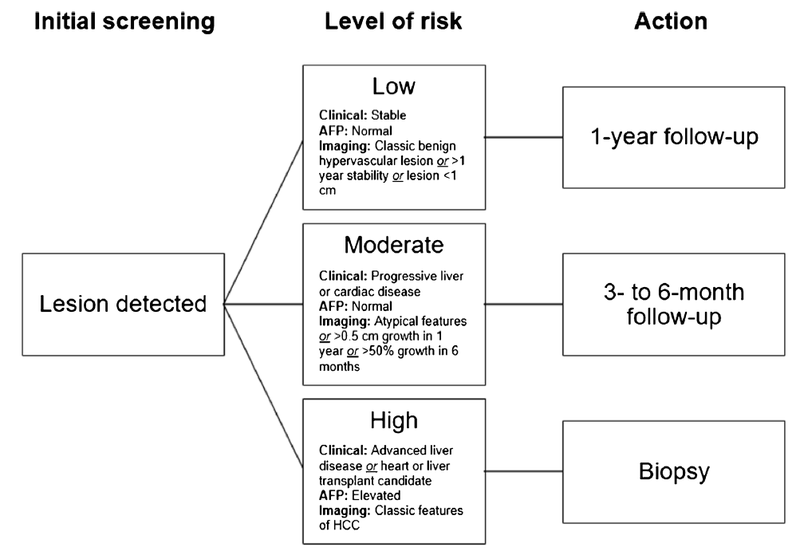
The Fontan operation is the third step in a series of surgeries to palliate single ventricle congenital heart disease (such as tricuspid atresia, mitral atresia, hypoplastic left heart syndrome). The first and second steps are the Norwood and bidirectional Glenn operations respectively, which serve to make a superior cavopulmonary connection. The Fontan operation then creates a surgical shunt to divert blood from the IVC and SVC to the pulmonary arteries (see Figure below). This operation is typically performed in children aged 2-5 years. In the US currently > 900 Fontan operations are performed each year, with 97% early survival rate!
Figure 1 - Diagram of Fontan circulation
Taken from: Gordon-Walker TT, et al. Fontan-associated liver disease: A review. J Cardiol. 2019
How is the liver affected during this process?
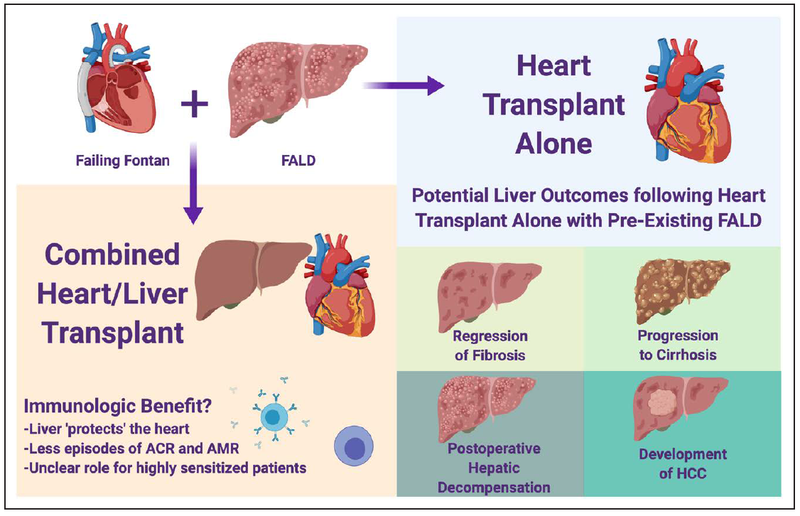
Fontan associated liver disease (FALD) is multifactorial- stemming from issues preoperatively, intraoperatively, and postoperatively. Prior to Fontan correction, single ventricle physiology may cause hepatic insults from hypotensive crises and relative ischemia. The series of stages cardiac surgeries can lead to additional ischemic insults to the liver. After completion of the surgeries, Fontan physiology leads to chronically elevated central venous pressure, decreased pulsatility in the hepatic veins, and frequently decreased cardiac output, and passive hepatic venous congestion. As a result of decreased cardiac output and hypoxemia, there is decreased oxygen delivery to centrilobular hepatocytes (zone 3). Hepatic venous congestion leads to reactive fibrogenesis – centrilobular hepatocyte atrophy, sinusoidal fibrosis, bridging fibrosis and ultimately cardiac cirrhosis.
Figure 2 - Mechanisms of liver injury in FALD,
Taken from: Gordon-Walker TT, et al. Fontan-associated liver disease: A review. J Cardiol. 2019
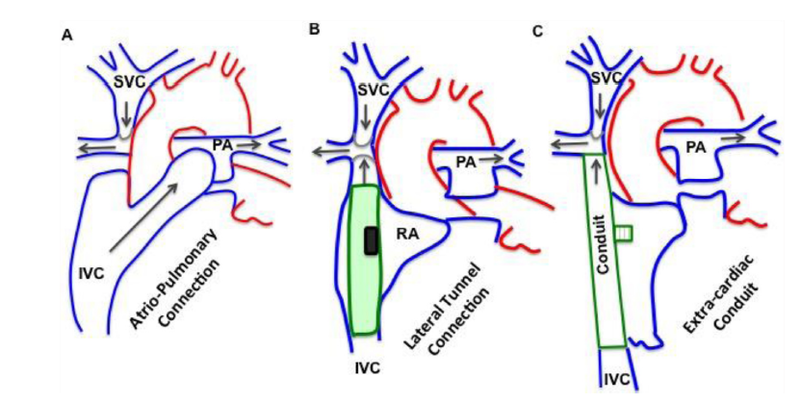
Liver fibrosis on biopsy is nearly universal in Fontan patients at 10 years or more postoperatively.5 The remaining challenge is determining how to screen for liver disease in these patients, as it is often clinically silent. FALD also increases the chances of developing liver lesions, from focal nodular hyperplasia, adenomas, to even hepatocellular carcinoma, which can unfortunately be seen in pediatric patients.
Figure 3 -Algorithm for monitoring detecting focal lesions in FALD
Taken from: Dillman JR et al. Imaging of Fontan-associated liver disease. Pediatr Radiol. 2020
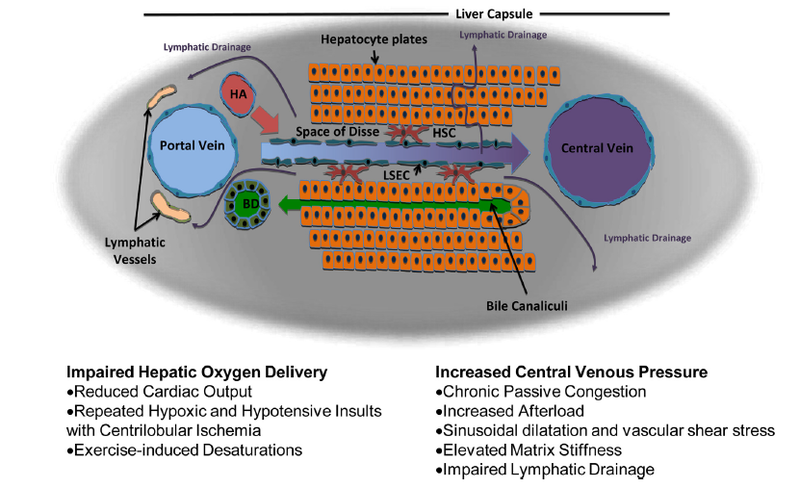
Recommendations for Transplantation: Heart Alone vs Heart-Liver
In patients who have a failing Fontan, we are faced with the question of heart transplant alone vs a combined heart and liver transplant (CHLT). This is obviously a complicated topic that we will only touch on briefly in this post. There is some evidence to suggest that FALD may stabilize after heart transplant alone; however, the risk of HCC remains. Data from Stanford, UCLA, Mayo Clinic, and the University of Pennsylvania support decreased rates of acute cellular rejection following as compared to episodes of acute cellular rejection in patients who received isolated heart transplants. The degree of immune allosensitization in Fontan patients may also make the immune benefits of CHLT appealing. CHLT may also be considered in patients who have developed HCC from FALD but may not have failing Fontan physiology.
Figure 4 -Considerations for CHLT vs Heart Transplant Alone