Hepatology casts a wide NET
Neuroendocrine neoplasms
Derived from enterochromaffin cells, neuroendocrine neoplasms (NEN) are a rare type of tumor. WHO 2019 classification categorizes NENs into well differentiated neuroendocrine tumors (NETs) and poorly differentiated neuroendocrine carcinomas (NECs). Tumor grading is based on mitotic rate and Ki-67 index with low grade having a low mitotic rate and Ki-67 index. These neoplasms are usually found incidentally on imaging or histopathology.
Gastrointestinal neuroendocrine tumors (NETs) commonly develop in the small intestine, stomach, rectum, and appendix. The most common location within the small intestine is the ileum, as in this patient. Most small intestinal NETs are well-differentiated and metastasize to the liver, lymph nodes, mesentery, bone, or lung. Most patients with small intestinal NETs present with intestinal obstruction, pain, weight loss and tumors in this location are commonly associated with carcinoid syndrome because they are drained by the portal vein. The 5-year survival of metastatic small intestinal NET is ~70% and largely dependent on stage at time of diagnosis. The presence of carcinoid syndrome or carcinoid heart disease is a prognostic factor for worse outcomes.
Carcinoid Syndrome
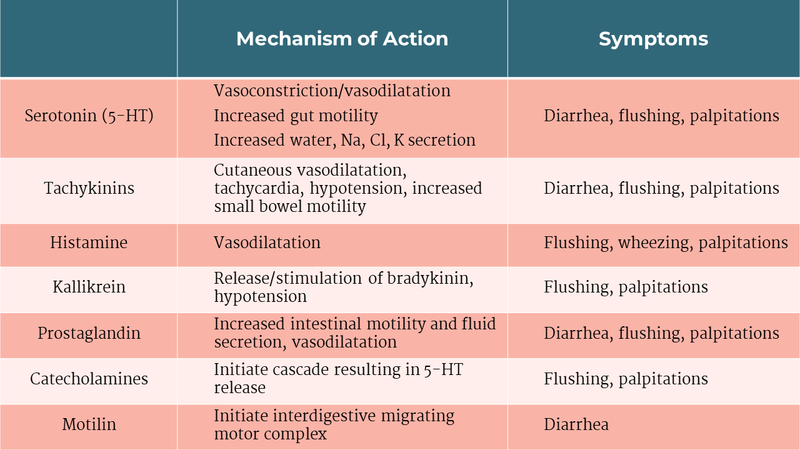
Some NETs produce hormones such as 5-HT, histamine, tachykinins, motilin, and kallikrein, resulting in a functional syndrome. Halperin et al noted that 19% of NET patients had carcinoid syndrome. Carcinoid syndrome is characterized by flushing, palpitations, secretory diarrhea, pellagra, and occasionally bronchospasm. Most cases of the classic carcinoid syndrome occur in the setting of hepatic metastases as these tumors can bypass hepatic inactivation of hormones but can also occur in patients with retroperitoneal lymph node metastases, primary ovarian, or primary pulmonary tumors.
Table 1: Molecules and symptoms of carcinoid syndrome.
EVALUATION
Laboratory Testing
Chromogranin A level (sensitivity 93% and specificity 85% via radioimmunoassay) should be obtained in the evaluation of and in follow up of a NET. Patients suspected of having carcinoid syndrome should be evaluated with a 24-hour urinary 5-HIAA (sensitivity and specificity > 90%) and the degree of elevation correlates with tumor burden.
Endoscopy & Imaging
Endoscopy allows for histopathologic examination in which the specimen will be synaptophysin and chromogranin A positive arranged in a well-developed shape. Staging with contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) is also recommended. MRI is more sensitive for hepatic metastases than CT.
Somatostatin receptor scintigraphy provides information on staging, occult lesions, and the expression of somatostatin receptors thereby evaluating into the candidacy of somatostatin analogue therapy. The two imaging modalities available are indium-pentetreotide (octreotide scan) and PET/CT gallium imaging using edotreotide which has greater sensitivity. Literature suggests that a Ga-dotatate scan is the most high-yield imaging test available.
Figure 1: Diagnostic algorithm in the evaluation of a neuroendocrine neoplasm.
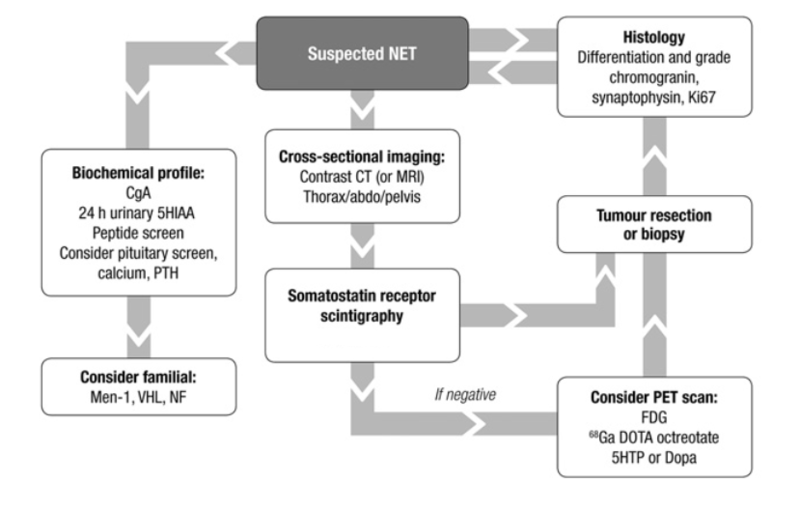
Image taken from: Guidelines for the management of gastropancreatic neuroendocrine (including carcinoid) tumors (NETs). Gut. 2012.
TREATMENT
Surgical
Resection of the primary NET and regional lymph nodes is preferred because reduction of NET burden improves symptoms (less hormone production), reduces the risk of bowel obstruction, and may allow subsequent therapies. When 90% of hepatic metastases can be resected, cytoreductive hepatic surgery is possible and carries a 5-year survival rate of 75-80%. However, recurrence rate in the remnant liver is elevated. This type of surgery may be necessary in patients with refractory symptoms and inability to lower 5-HT levels.
Liver directed treatment
Liver-directed therapies including ablation, hepatic artery embolization and chemoembolization, hepatic radioembolization are options in patients with unresectable disease. One single-center study looked at both bland and chemoembolization of the hepatic artery and 63% of patients had symptom reduction with a median progression-free survival of 19 months for those enrolled.
Role of transplantation
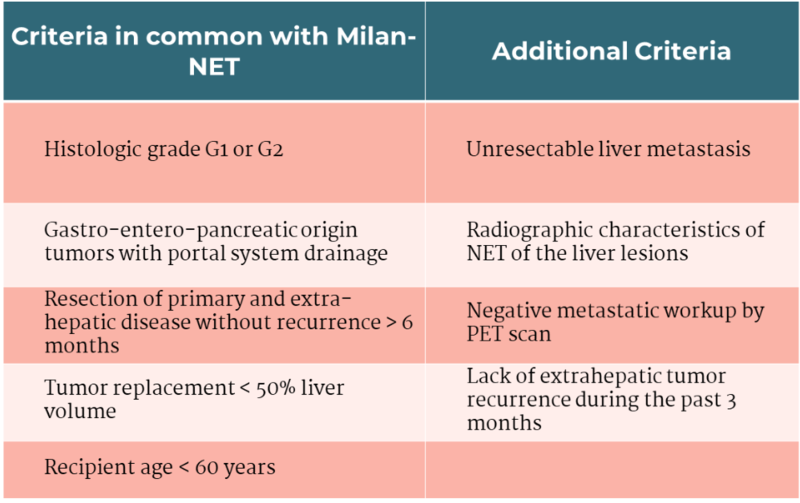
The Organ Procurement and Transplant Network may grant transplant exception points for candidates with low-grade, well-differentiated gastro-entero-pancreatic origin NETs who are < 60 years old, have undergone resection of the primary tumor and extra-hepatic disease without evidence of recurrence for at least six months (surveyed with imaging), and have unresectable liver metastases. Further criteria are shown in Table 2. Patients with a primary tumor in the rectum, esophagus, lung, thyroid, and adrenals are not candidates for model for end-stage liver disease (MELD) exception as these locations are not drained by the portal venous system. Patients with extra-hepatic solid organ metastases are not eligible as well. Surveillance workup should be performed every 3 months for MELD exception.
Table 2: United Network for Organ Sharing criteria for liver transplantation in NET.
Liver transplantation is an option in a select population with well-differentiated disease. One study compared a cohort who underwent transplant against a nontransplant treatment. There was a significant difference in overall survival at 5-years and 10-years in the transplant group compared to the nontransplant group. It is important to note that the patients enrolled into the transplant arm were < 60 years old, had low-grade NET which was drained by the portal venous system, underwent resection of the primary tumor and extrahepatic metastases, had < 50% of total liver volume involved, and had 6 months of surveillance without disease progression. A multicenter retrospective study determined a 5-year overall survival of 59%. The group identified the following risk factors for worse outcomes: age > 45 years at time of transplant, primary tumor from the pancreas, hepatomegaly, lymph node involvement, positive resection margins, and resection of primary tumor at time of transplant. NET recurrence post-transplant can occur and analysis of registries showed a rate ranging from 31.3-56.8% with variable time to recurrence. These patients should be followed in a surveillance program which includes imaging and monitoring chromogranin A levels.
Medical Treatment
These patients should be referred to Oncology for treatment considerations.
Somatostatin analogues are the treatment of choice for carcinoid syndrome. Depot injections provide sustained control of symptoms for a vast majority of patients. They also inhibit tumor growth via an unknown mechanism. The PROMID trial showed a significant improvement in median time to progression with octreotide LAR and the CLARINET trial showed improved progression-free survival with lanreotide. Patients should be counseled about adverse events including cholelithiasis formation, steatorrhea, bradycardia. Telotristat is a tryptophan hydroxylase inhibitor and can be used in patients with refractory diarrhea. The mTOR inhibitor everolimus can also be used for refractory flushing and diarrhea. Peptide receptor radionuclide radiotherapy (PRRT) with 177-lutetium-dotatate can also be considered in combination with somatostatin analogue therapy and it was shown to significantly improve progression-free survival. This therapy utilizes cytotoxic radiolabeled somatostatin receptor ligands to target tumors directly.
Chemotherapy is generally reserved for patients in which no other treatment modalities are feasible. Poorly differentiated tumors (NECs) tend to be somatostatin receptor poor and somatostatin analogues and PRRT are not options. These patients tend to have diffuse disease at presentation. Systemic chemotherapy with platinum-based regimen is the treatment of choice and 5-year survival is only 11%. There is data supporting the use of immunotherapy in poorly differentiated NENs as well and further investigation is necessary.
Figure 2: Treatment algorithm in the evaluation of a neuroendocrine neoplasm.
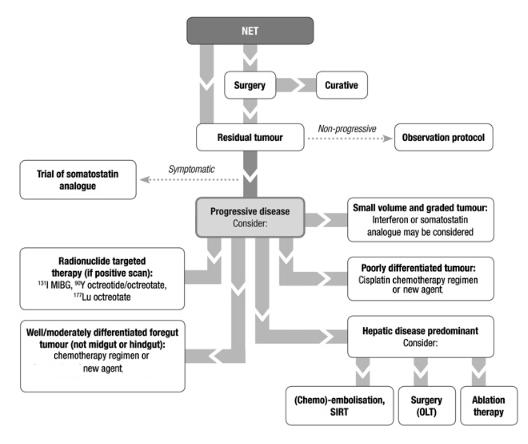
Image taken from: Guidelines for the management of gastropancreatic neuroendocrine (including carcinoid) tumors (NETs). Gut. 2012.