It Takes Two: Liver diseases of pregnancy
Background
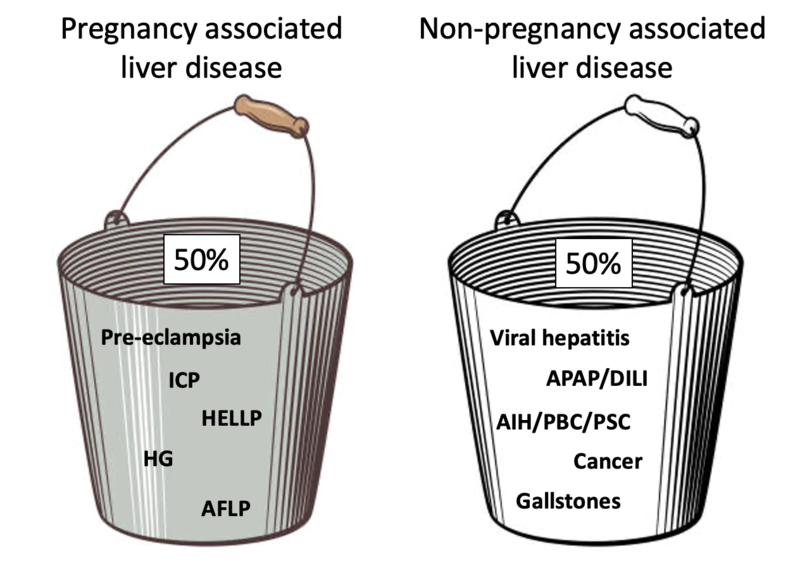
Let’s start by dividing up liver disease in pregnancy into two buckets: liver disease that just-so-happens to occur during pregnancy, and liver diseases that are directly related to pregnancy itself. About half of cases fall into each of these two groups. Although we’ll focus on the latter group in today’s post, it’s important to remember the adage that “common things are common.” After all, the top cause of acute liver failure in pregnancy is acetaminophen toxicity, accounting for 30% of cases! Also keep in mind that physiologic changes of pregnancy cause alterations in normal liver tests (see a prior post for more details).
Not-so-fun fact: gallstones can be seen in up to 10% of pregnant patients. Hormonal changes decrease gallbladder contractility and promote formation of gallbladder sludge. Ultrasound can be safely performed to evaluate.
Liver diseases of pregnancy
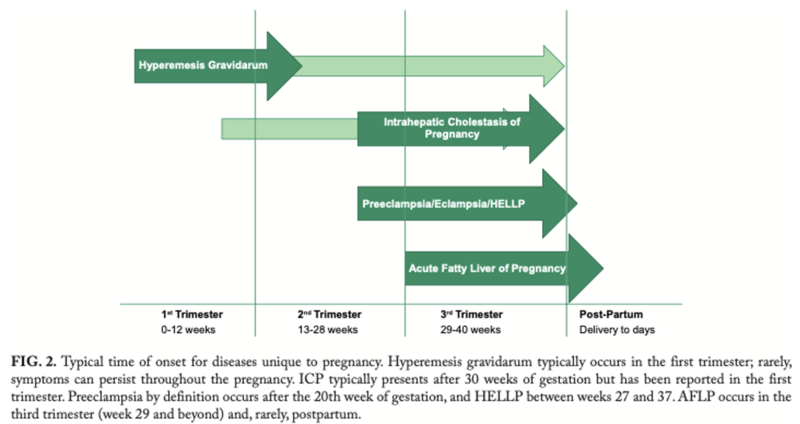
Now we’ll focus our attention on liver diseases unique to pregnancy. Much is still unknown about these disorders, and there is significant overlap in pathophysiology and clinical presentation. In fact, pre-eclampsia, HELLP, and AFLP may represent a spectrum of disease with a common predisposition, and further research is ongoing. A helpful framework for these disorders is pictured below categorized by trimester.
Hyperemesis Gravidarum
In contrast to nausea and vomiting of pregnancy which is present in about half of pregnancies, hyperemesis gravidarum is defined by severe symptoms causing loss of ≥5% of pre-pregnancy body weight and occurs in up to 2% of pregnancies, generally limited to the first trimester (although 20% have symptoms throughout pregnancy). The cause may be genetic and occurs more frequently in molar and multifetal pregnancies and those with underlying endocrinopathies. The associated hypovolemia can cause electrolyte disturbances and ketonuria, which generally resolve with fluid resuscitation. Liver involvement is seen in 50% of cases due to a starvation state, with ALT>AST although both are usually less than 1,000 U/L. Treatment includes rehydration, vitamin and nutritional supplementation, and supportive care with anti-emetics. Rarely, enteral or parenteral nutrition is needed. Adverse fetal outcomes including growth restriction are associated with poor maternal weight gain, although this risk is mitigated with adequate hydration and nutrition.
Intrahepatic cholestasis of pregnancy
See a prior LFN post for more information on ICP.
Hypertensive disorders of pregnancy: pre-eclampsia, eclampsia, and HELLP syndrome
Hypertensive disorders of pregnancy are a major cause of maternal and fetal morbidity and mortality. Pre-eclampsia or eclampsia affect up to 8% of pregnancies, with rising rates due to increased risk factors including increased maternal age and metabolic syndrome. Up to 20% of patients with pre-eclampsia or eclampsia develop comorbid HELLP syndrome.
Pre-eclampsia and eclampsia
Although the exact pathophysiology for pre-eclampsia is debated, it likely is due to abnormal placentation causing decreased placental blood flow, cytokine release, and endothelial dysfunction. It is defined by new-onset hypertension (>140/90 mmHg) or proteinuria (>30mg/day or ≥1+ protein on dipstick) after 20 weeks gestation, with multi-organ involvement as seen below. Eclampsia is defined by severe neurologic involvement causing seizures; magnesium sulfate may help prevent this. Patients may be asymptomatic, or present with headache, blurry vision, abdominal pain, nausea/vomiting, or edema.
ACOG recommends low-dose aspirin for prevention in high-risk women starting prior to 16 weeks gestation through delivery. Planned early delivery should be considered around 37 weeks with guidance from our obstetrical colleagues. Women have an increased future risk of pregnancy complications and cardiovascular disease.
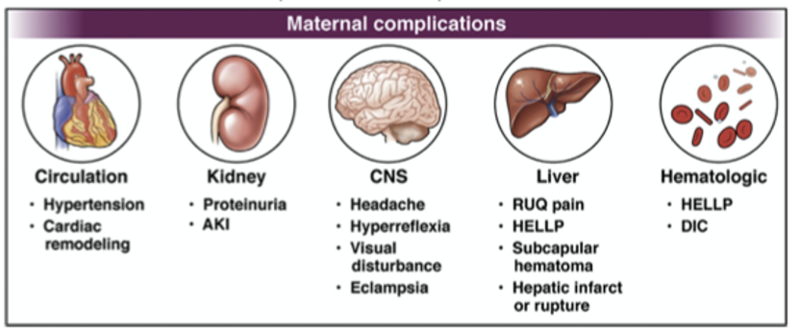
HELLP syndrome (hemolysis with elevated liver enzymes and low platelets)
Placental hypoperfusion leads to a release of cytokines, activation of the coagulation cascade, and resulting microangiopathy and endothelial dysfunction. This causes the titular lab abnormalities due to shear stress from systemic microthrombi and hepatic hypoperfusion. Patients with comorbid pre-eclampsia and HELLP have worse outcomes: maternal mortality is up to 10% and perinatal mortality up to 15%, owing to higher rates of placental abruption, acute renal failure, and DIC. Acute liver failure is reported to occur in 4.5% of patients with HELLP, and more rarely, hepatic rupture and hemorrhage can occur.
Acute fatty liver of pregnancy (AFLP)
The etiology of AFLP is likely due to abnormal fatty acid oxidation. This may be due to infant inborn errors of metabolism in the setting of increased plasma triglycerides and free fatty acids late in pregnancy, explaining its predominance in the third trimester. Up to 25% of cases occur post-partum, and the Swansea Criteria can aid in diagnosis.
Swansea criteria for diagnosis of AFLP (6+ criteria support a diagnosis)
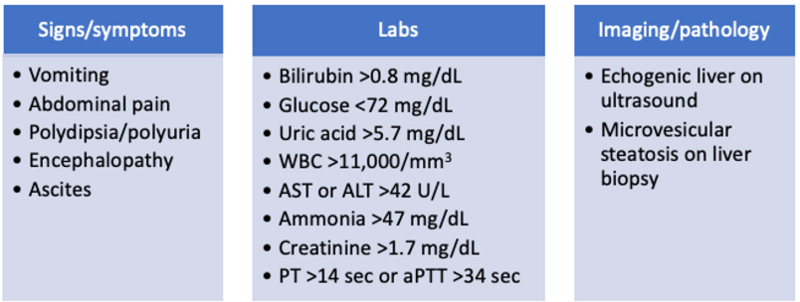
The risk of maternal mortality corresponds to the MELD score, with the highest rate of complications occurring in those with a MELD >30. ACOG guidelines recommend prompt delivery by vaginal delivery or Cesarean section, and consideration of liver transplantation in those with evidence of liver failure. Improvement is generally seen in the first week after delivery, and the need for liver transplant is rare. Infants should be referred to genetic counseling for consideration of screening for disorders of fatty acid oxidation.
Stay tuned for the next post in our Reproductive Health series, which will focus on contraception, pre-conception counseling, and management of chronic liver disease in pregnancy.