Acute hepatitis in pregnancy – the truth is more than skin deep
Herpes Simplex Virus (HSV) Hepatitis – Clinical Presentation
- While HSV is a rare cause of acute liver failure, representing less than 1% of all cases of acute liver failure, the diagnosis has an extremely high mortality rate approaching 75%.
- HSV hepatitis most commonly affects immunocompromised patients, including pregnant women, patients receiving immunosuppressant agents, and patients with HIV/AIDS, though HSV hepatitis can also occur in immunocompetent patients.
- HSV seroprevalence is high in women of child-bearing age in the United States (60% HSV-1, 20% HSV-2). In pregnant women, HSV hepatitis can have a fulminant course with maternal mortality approaching 40%.
- Common features of HSV hepatitis are fever, upper respiratory infection symptoms, an anicteric hepatitis with very high ALT/AST, leukopenia, and thrombocytopenia.
- The pathognomonic mucocutaneous lesions of HSV are only present in less than 50% of cases.
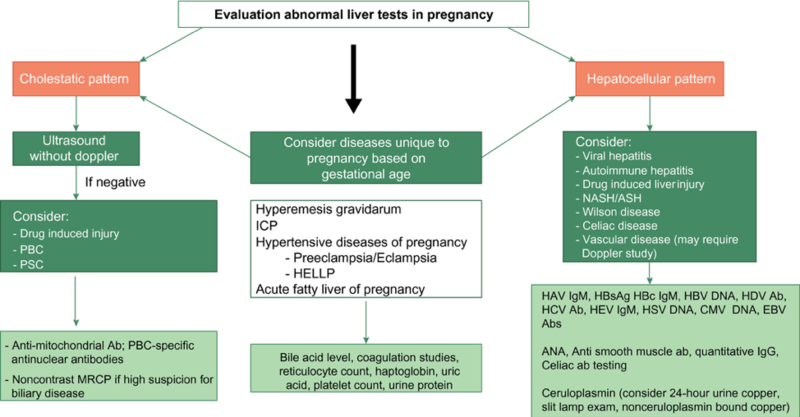
Two great reviews of acute hepatitis in pregnancy can be seen in the 2015 ACG Clinical Guideline: Liver Disease and Pregnancy and the 2020 AASLD Practice Guidance: Reproductive Health and Liver Disease (see Figure 1).
Figure 1: Evaluation of abnormal liver tests pregnancy
HSV Hepatitis – Diagnostics
- The diagnosis of HSV is frequently made postmortem so clinicians should maintain a high degree of clinical suspicion for the diagnosis
- HSV-IgM testing has limited specificity and sensitivity, so HSV PCR should be performed when HSV hepatitis is suspected as detection of HSV DNA appears to be more discriminating than serological testing for diagnosing or excluding HSV as a cause of acute liver failure.
- For centers in which HSV PCR testing is not rapidly available, a liver biopsy via a transjugular approach may be needed for definitive diagnosis if safe to do so (see Figure 2).
Figure 2: HSV hepatitis on liver biopsy

Taken from: WebPathology – Visual Survey of Surgical Pathology, Herpes Simplex Virus Hepatitis.
HSV Hepatitis – Treatment
- High dose IV acyclovir should be started once HSV hepatitis is suspected.
- Acyclovir has been shown to be safe and well-tolerated in pregnancy and during lactation.
- Early acyclovir treatment is associated with improved outcomes in HSV hepatitis including improved mortality and reduced need for liver transplantation
- The duration of anti-viral therapy is unclear but should be guided by clinical factors such as improvement in liver enzyme tests, negative serum PCR, and improvement in symptoms
- Acyclovir-resistance should be considered in patients who are not improving on acyclovir therapy, and use of additional agents such as foscarnet should be considered under the guidance of infectious disease consultation