Pediatric Liver Transplant Prioritization
Why is pediatric prioritization important?
Ethical considerations
Before discussing how pediatric patients are being prioritized on liver transplant waitlists, it is important to discuss the ethical justifications for why children should be prioritized. Globally, there have been a few pivotal declarations calling for the protection of the rights of children. First, in 1924, the League of Nations published The Declaration of the Rights of a Child which states that “mankind owes to the child the best that it has to give”. In 1959 the United Nations General Assembly approved a resolution to protect the rights of children. This resolution stated that children should have special protection and be given opportunities by law and by other means, to enable them to develop physically, mentally, morally, spiritually, and socially in a healthy and normal manner.
Now to focus in on how the protection of the rights of children is modeled through pediatric prioritization in liver transplant. In 2014, the United Network for Organ Sharing published four ethical principles supporting the need for pediatric prioritization. 1. Prudential life span: when resources are limited, the resources should be allocated to those with the greatest potential benefit over time. 2. Maximin principle: resources should be allocated to the most vulnerable to give the greatest benefit to the most disadvantaged. 3. Utility: children have superior survival rates and longer survival in comparison to adults. 4: Fair innings: everyone deserves to live a full life and a child’s premature death would lead to a greater number of years lost. Hernandez Benabe et al. stated “The argument of prioritizing patients under 18 years of age in allocation is not only based on the advocating for the rights of children but also in addressing waitlist mortality and timeliness of transplantation, particularly for the youngest, smallest, and sickest”
Waitlist mortality
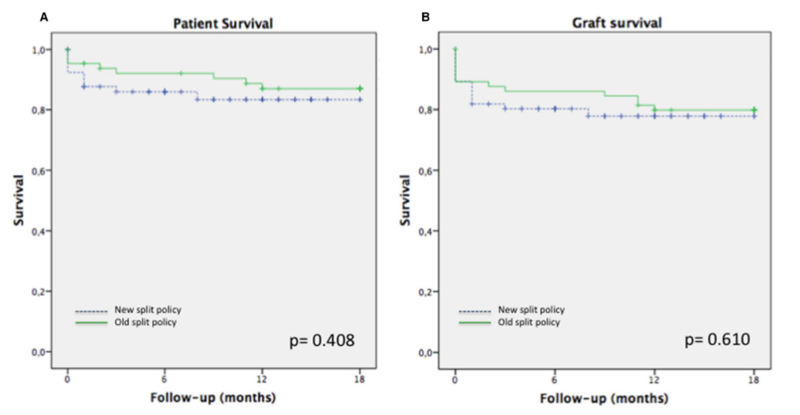
Despite efforts to prioritize children in organ allocation, pretransplant mortality rates have only slightly improved over the past few years in the US. The most recent pretransplant pediatric mortality rates reported by Organ Procurement & Transplantation Network (OPTN)/Scientific Registry of Transplant Recipients (SRTR) in 2021 at 5.6 deaths per 100 patient-years and highest amongst children younger than 1 year of age at 21.7 deaths per 100 patient-years (Figure 1). Prolonged waitlist times do not only increase waitlist mortality, but may also lead to compromise of nutrition, cognitive, and social development increasing lifetime morbidity.
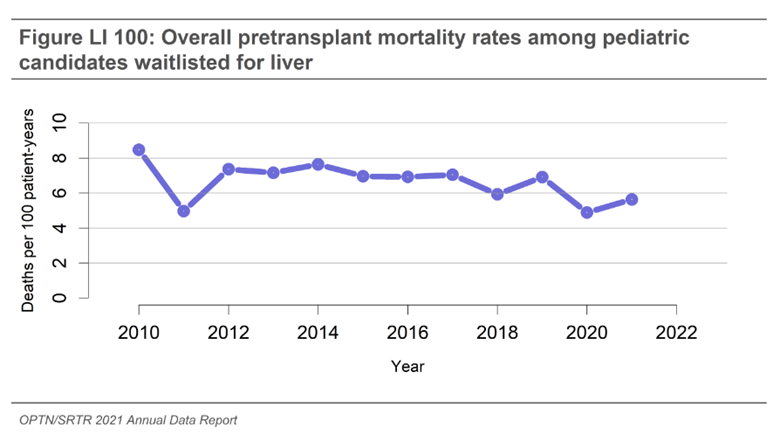
Figure 1: OPTN/SRTR 2021 report pediatric pretransplant mortality rates
Pediatric Prioritization in the US
Prior to 1997 patients on the waitlist were allocated organs within their local organ procurement organization (OPO) based on two criteria: 1. their location, whether in the hospital, intensive care unit, or home, and 2. accrued waitlist time. To address US congress mandates for objective ranking on the waitlist, MELD and PELD scores were implemented in 2002 and with the goal to represent risk of mortality in the next 3 months. The MELD score is used for adults and children 12 years and older, and the PELD score is used for children under 12 years old. The initial calculations were slightly different with MELD comprised of creatinine, total bilirubin, and INR and PELD of total bilirubin, INR, albumin, age less than 1 year, and growth failure . Multiple studies using national registry data have been published indicating the PELD score in fact underrepresents the risk for wait-list mortality for children in comparison with adults, and therefore the PELD score did not prioritize children accurately. As a result, standardized exceptions were outlined to allocate a specific number of extra points in addition to the calculated PELD/MELD score, for example for certain metabolic liver diseases. In addition, non-standardized exception points could be awarded on a case-by-case basis for complications not represented in the PELD such as poor growth, infection, or portal hypertension. This led to a large proportion of children being listed with either standardized or non-standardized exception points with 34% of children between 2002 and 2013 being listed with a non-standardized exception request at the time of transplant. In 2020 61% of children were listed with an exception MELD or PELD score. While exception points help to prioritize children on the waitlist, it was not standardized and there was significant variation in approval by region, race, and insurance status. While initially non-standard exceptions were evaluated regionally, in 2019 the national liver review board was developed by United Network for Organ Sharing (UNOS) to review non-standard exception point approvals.
In 2000 a policy was implemented for children listed with highest priority status to be given priority for pediatric donor livers. Despite this, 45% of pediatric donor livers between 2010-2014 were allocated to adults. A new policy was implemented in February 2020 that replaced donor service areas with “acuity circles”, which are concentric circles measured in nautical miles around the donor hospital replacing. This policy also outlined prioritization of pediatric livers be offered to pediatric recipients nationally prior to offering the liver to an adult locally. The true impact of this change is yet to be seen given the onset of this change at the beginning of the COVID-19 pandemic, though initial data shows lower pediatric waitlist mortality in 2020 and 2021 while adult waitlist mortality rates remained stable.
The most recent OPTN Policy changes occurred in July 2023 and one focus of these policy changes was to improve the PELD score representation of waitlist mortality risk. This new PELD Cr adds creatinine to the score calculation, as well as age-adjusted mortality risk to better align pediatric and adult scores with true mortality risk. Status 1B was implemented in 2007 to improve priority for children with acute on chronic liver failure (ACLF). Unfortunately, in comparison to children listed 1A with acute liver failure and 1B with non-ACLF, children with ACLF listed status 1B have the highest rates of mortality both pre- and post- transplant and the lowest rates of transplant. There were also recent changes in 2023 to 1B to better capture children with acute liver failure and acute on chronic liver failure including removal of the requirement of calculated MELD/PELD≥25 to qualify for Status 1B . Given its recent implementation, the results of these changes on pediatric prioritization and waitlist mortality have not yet been evaluated.
International approaches to pediatric prioritization
The need for pediatric prioritization in liver transplant has been recognized internationally, but methods of promoting pediatric prioritization in liver transplantation vary widely.
Organ Allocation
Many countries have taken similar approaches in prioritizing pediatric donors to pediatric recipients. Some countries that have implemented these policies include Australia, New Zealand, Argentina, France, United Kingdom, Japan, and Scandiatransplant network. Some countries have taken this a step further and also prioritize pediatric recipients for adult donors meeting certain criteria. For example, after allocation to emergency recipients, all donors aged 18 to 50 in Italy and 16 to 35 years in Spain are prioritized to pediatric recipients. Prioritization of adult livers to pediatric recipients also encourages splitting of livers as many small children will only receive the left lateral segment, increasing the organ availability to both pediatric and adult recipients.
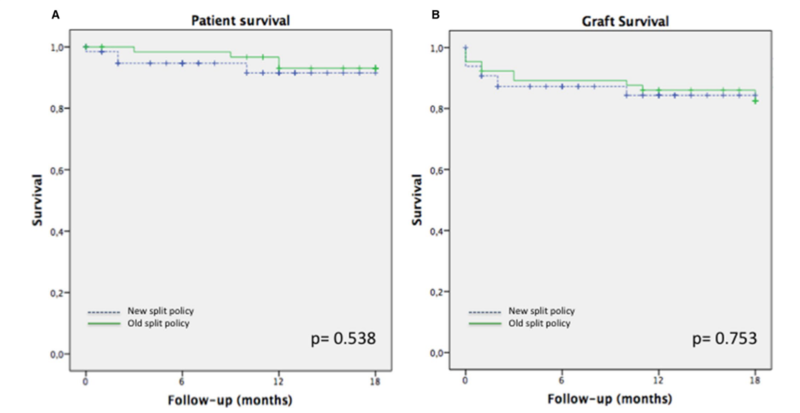
Some countries or transplant networks including United Kingdom, France, Italy, Scandiatransplant, and Eurotransplant have instated policies regarding splitting livers. While there are many nuances to the policy, the goal is to increase the donor pool while also prioritizing the use of the left lateral segment to pediatric recipients by mandating splitting appropriate donor livers. In the United Kingdom, 4 years after implementation of their “intention to split” policy, no children died on the waitlist. Eurotransplant saw an increase in liver splitting and decreased pediatric waitlist mortality by 36%. In Italy, after the implementation of their splitting policy, transplantation of split grafts increased from 49% to 66% in children and waitlist time significantly reduced from 229 days to 80 days. They also saw a decrease in both pediatric waitlist mortality from 4.5% to 2.5% as well as adult waitlist mortality from 9.7% to 5.2%. These improved outcomes with implementation of splitting policy did not lead to decreased patient or graft survival in those receiving either left lateral segments (Figure 2) or extended right grafts (figure 3).
Figure 2: Patient survival (A) and graft survival (B) in those receiving left lateral segments. Angelico et al, 2019
Figure 3: Patient survival (A) and graft survival (B) in those receiving extended right grafts. Angelico et al, 2019.
While the US has implemented a policy encouraging, but not mandating the splitting of livers meeting certain criteria, it has not led to the increase in split utilization.
Score augmentation
A different approach to prioritization of children are mechanisms for assigning them higher objective PELD or MELD scores to place them in front of adult patients. In Canada and Eurotransplant, pediatric patients are assigned higher baseline scores by various methods and then have incremental increases in their score every 90 days that they remain on the waitlist. For example, in Eurotransplant, children under 2 years with biliary atresia are given a MELD of 32 and every 90 days it is increased by 15%. In Brazil, a dramatic take on prioritization was implemented where the PELD score for all children under 12 years of age is multiplied by 3 and children over 12 the MELD is multiplied by 2. This led to universal prioritization of children placing them higher than adults on the waitlist without changing the order between children. The result of this policy led to a significant decrease in waitlist time for children from 20.3 to 2.7 months.
Take home points
- We have an ethical responsibility to improve pediatric prioritization in liver transplant
- The US has made many changes over time to improve pediatric prioritization, the results of the most recent changes in 2023 are yet to be evaluated
- Internationally children have been prioritized in unique manners including prioritization for both pediatric and adult donors as well as augmenting listing scores to better represent the mortality risk and overall increase pediatric listing scores