Pathology Pearls: Graft-Versus-Host Disease (GVHD)
Brief Case Presentation
A 40-year-old patient with a history of acute myeloid leukemia status post allogenic stem cell transplantation is admitted from clinic with jaundice and watery diarrhea. Select laboratory values are as follows:
| Lab Test | Result |
| AST | 52 U/L (0 – 39 U/L) |
| ALT | 119 U/L (0 – 52 U/L) |
| Alk. Phos | 552 U/L (49-139 U/L |
| Total Bilirubin | 1.4 mg/dL (0.2 – 1.2 mg/dL) |
| Albumin | 3.9 g/dL (3.5-5.7 g/dL) |
A liver biopsy was subsequently performed.
Liver Core Biopsy Findings
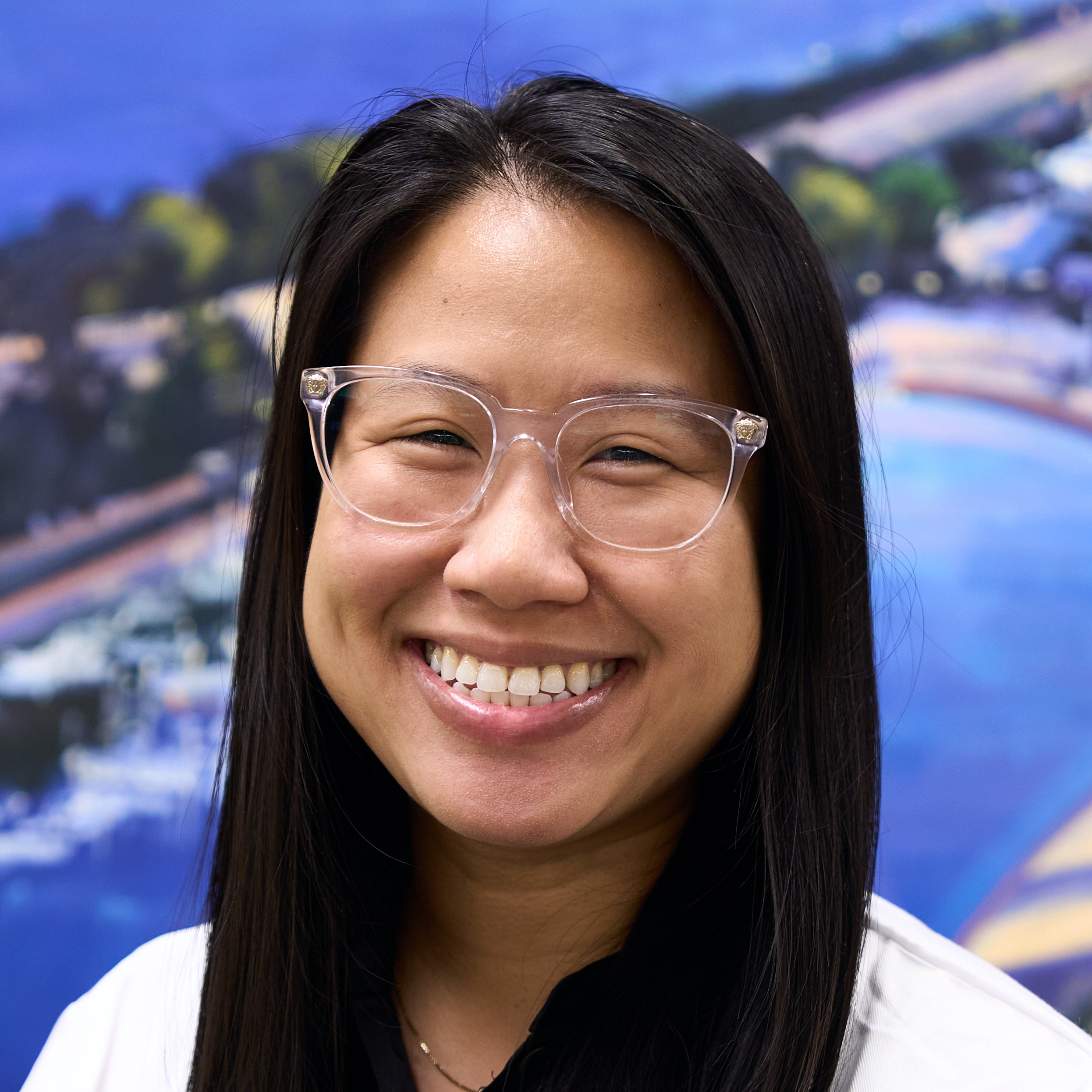
At low power, the liver core biopsy shows overall minimal lobular and portal inflammation (Figure 1).
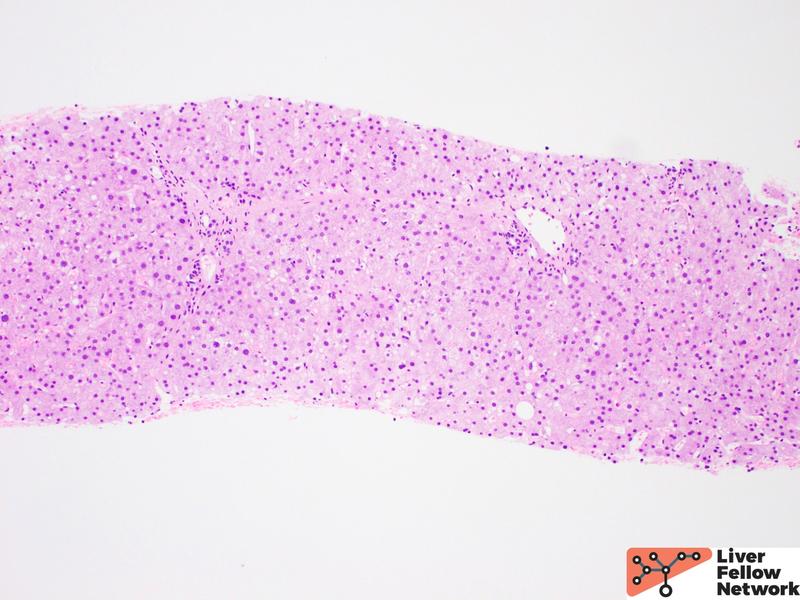
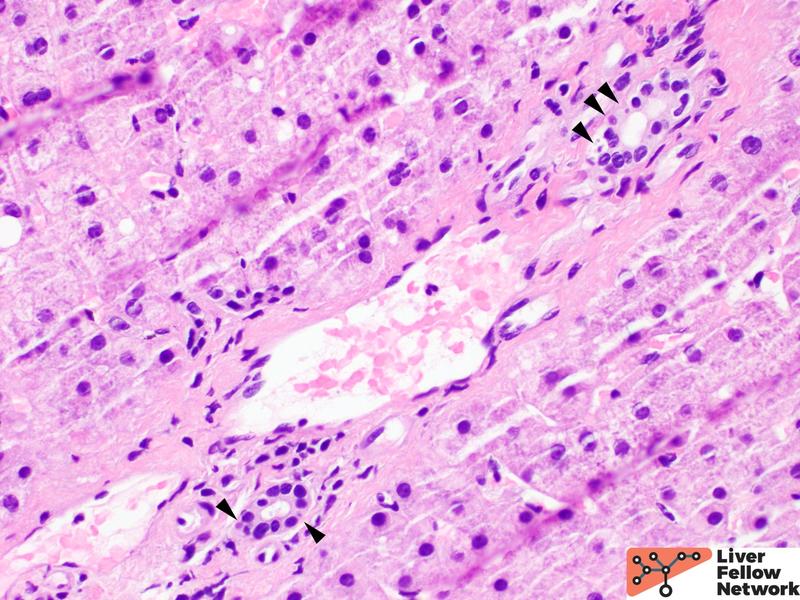
On higher power, some portal tracts show injured bile ducts. The biliary epithelial cells are irregular and unevenly spaced with cytoplasmic vacuolization and occasional apoptotic bodies (Figure 2 & 3).
In the clinical context provided, the histologic findings are compatible with hepatic graft-versus-host disease (GVHD).
Graft-Versus-Host Disease (GVHD)
GVHD is an immune-mediated complication that can develop in up to 70% of hematopoietic stem cell transplant (HCT) recipients and rarely in solid organ recipients and other immunosuppressed conditions. Historically, GVHD was classified as acute and chronic forms based on if disease occurred less than or greater than 100 days following HCT. Now, it is defined based on clinical features. Acute GVHD typically occurs within three weeks to three months following HCT and generally affects the skin, gastrointestinal tract, and liver. Patients with chronic GVHD tend to present with more generalized systemic manifestations involving salivary glands, lungs, lymph nodes, eyes, mouth, and musculoskeletal system. Isolated hepatic GVHD has been reported in approximately 1% of cases. Patients with hepatic GVHD most commonly present within three weeks to three months following HCT with jaundice and hepatomegaly. Laboratory testing may show elevated serum alkaline phosphatase and bilirubin with or without transaminitis.
GVHD results from immune-competent, donor-derived T-cells that are infused from the HCT (graft) recognizing recipient tissue antigens (host) as foreign/”not self”. This leads to T-cell activation with excess cytokine production and subsequent end-organ damage. Due to the recipient’s immunosuppressed state, these T-cells cannot be effectively destroyed or inactivated. Therefore, the most important risk factors for the development of GVHD are unrelated donor and HLA mismatch transplants.
The acute hepatitis pattern of GVHD can mimic other causes of acute hepatitis especially infection. Viral hepatitis can show diffuse lobular inflammation with hepatocellular injury (hepatocyte swelling, scattered acidophil bodies, or confluent necrosis). Mild portal and periportal inflammation with bile duct injury may be seen. Systemic infections such as HSV, CMV, and adenovirus can also show variable degrees of lobular inflammation, hepatocellular necrosis, and mononuclear portal inflammation. Careful histologic evaluation for viral cytopathic effect, as well as immunohistochemical stains and serologies are useful in excluding an infectious etiology.
Differential Diagnosis
The differential diagnosis for bile duct injury seen in the typical pattern of hepatic GVHD is broad and can include drug-induced liver injury, cholangitis, sepsis, and biliary obstruction. Drug-induced liver injury can be due to several different medications (NSAIDs, antibiotics, immune checkpoint inhibitors, antiepileptics, etc.) and show cholangitic, cholestatic or ductopenic patterns. Thorough patient history and medication review is required.
Finally, if the patient received the transplant for a systemic illness, evidence of liver involvement by recurrent disease must also be excluded histologically and clinically.
References
- Burt, MacSween’s Pathology of the Liver: Seventh Edition. 2017.
- Torbenson, Surgical Pathology of the Liver. 2018.
- Torbenson, Atlas of Liver Pathology: A Pattern-Based Approach. 2019
- Salomao M, Dorritie K, Mapara MY, Sepulveda A. Histopathology of graft-vs-host disease of gastrointestinal tract and liver: an update. Am J Clin Pathol. 2016;145(5):591-603.