Pathology Pearls Post 6: Autoimmune Hepatitis (AIH)
Brief Case Presentation
| Lab Value | Result |
|---|---|
| AST | 257 |
| ALT | 297 |
| ALP | 124 |
| Total Bilirubin | 0.8 |
| HAV | Negative |
| HBV | Negative |
| HCV | Negative |
| ANA | 1:160 |
| AMA | Negative |
| ASM | Negative |
| IgG | Negative |
A 70-year-old female with history of hypertension and hypercholesterolemia presents for follow-up of asymptomatic hypertransaminasemia detected on routine lab work. She denies drug, alcohol, and herbal use. Her daily medications include aspirin (81mg), atenolol, atorvastatin, and hydrochlorothiazide. Results from her liver function tests and serologic studies are seen below:
Lab Value Results
Liver Biopsy
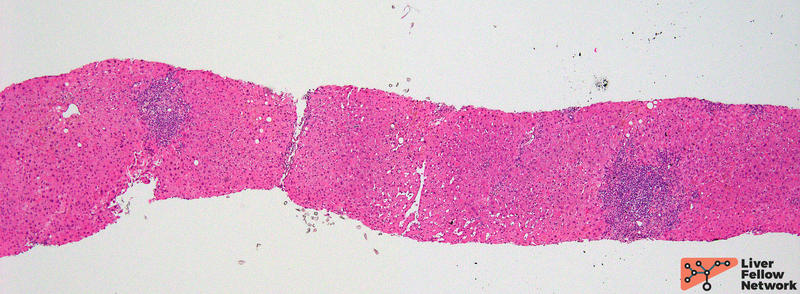
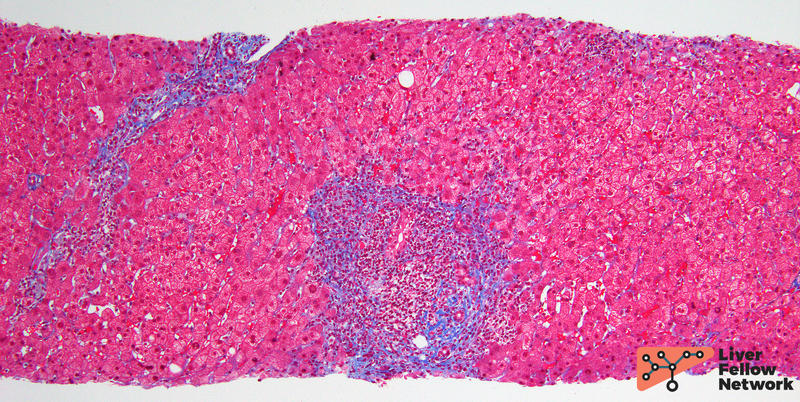
The patient is sent for a liver biopsy. At low magnification, the liver biopsy shows mild to moderate portal inflammation (Figure 1).
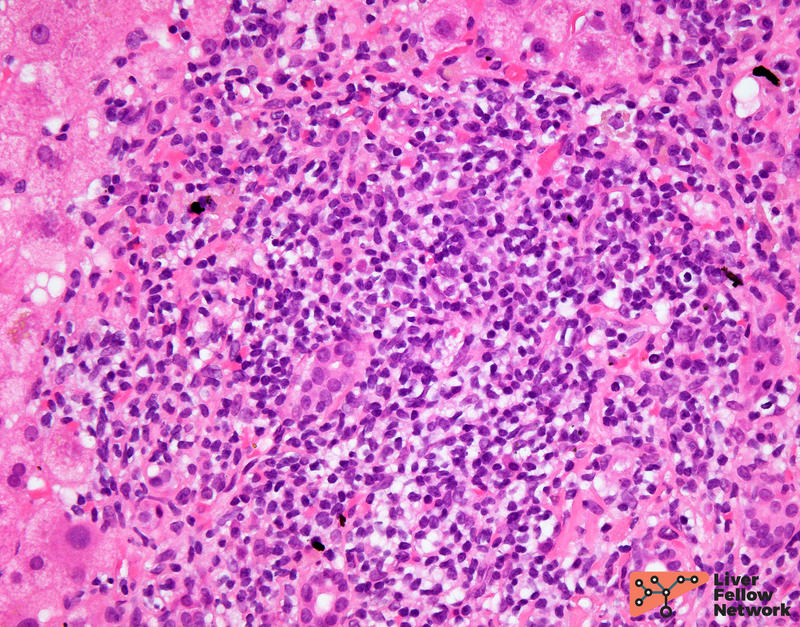
At higher power, the inflammation is predominantly lymphocytic and contains scattered plasma cells with occasional eosinophils (Figure 2).
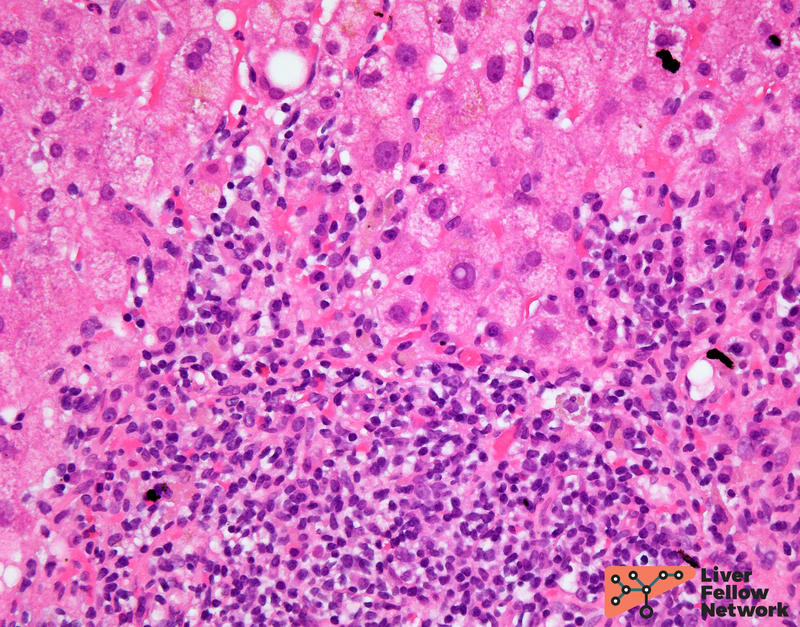
The native bile ducts are intact and mild interface activity is present (Figure 3).
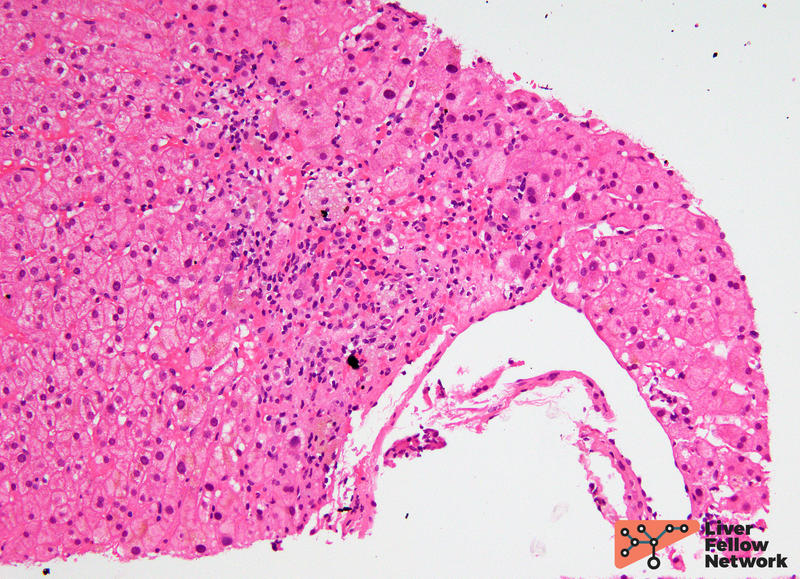
There is minimal lobular inflammation with rare areas of hepatocyte dropout (Figure 4).
A trichrome stains shows no significant increase in fibrosis (Figure 5).
In this clinical context, the histologic findings are most suggestive of autoimmune hepatitis (AIH) (Batts and Ludwig, grade 2, stage 0-1).
Histologic Features of AIH
A spectrum of histologic features can be seen in AIH, which is why correlation with clinical and laboratory findings is essential. Most commonly, AIH demonstrates a chronic hepatitis pattern of injury. The portal tracts show mild to moderate lymphocytic inflammation in the portal tracts, which is often rich in plasma cells. No bile duct injury or loss is seen. Interface activity is readily identified and is considered a characteristic feature of AIH; however, this can also be seen in viral hepatitis or drug/medication-induced injury. Lobular inflammation in the form of lymphocytes and plasma cells, as well as hepatocellular damage, may also be present.
AIH can progress to cirrhosis, thus it is also important to stage fibrosis in these liver biopsies (using Batts and Ludwig as described in our prior post): 0 = no fibrosis, 1 = portal fibrosis, 2 = portal and periportal fibrosis, 3 = bridging fibrosis, and 4 = cirrhosis.
It is important to note that some patients will receive steroids PRIOR to their liver biopsy, which may reduce the amount of inflammation seen in the liver biopsy (including plasma cells). In these cases, if the clinical picture is suspicious for AIH and other causes have been excluded, the histologic features can be designated "compatible with treated AIH."
Proposed Diagnostic Criteria for AIH
Like the histologic findings, the clinical presentation of AIH can also be quite variable. As such, the International Autoimmune Hepatitis Group created a scoring system that combines clinical and histologic variables to generate a score to predict the likelihood of AIH (Table 1)[4,5]. If the final score is ≥ 6, the patient has probable AIH, while a final score ≥ 7 is diagnostic for AIH.
Table 1. Simplified Diagnostic Criteria for Autoimmune Hepatitis
(adapted from Hennes et al.[4,5])
VariableCutoffPoints
| Lab Value | Cutoff | Points | |
|---|---|---|---|
| ANA or SMA | ≥1:40 | 1 | |
| ANA or SMA | ≥1:80 | ||
| or LKM | ≥1:40 | 2 | |
| or SLA | positive | ||
| IgG | > upper normal limit | 1 | |
|
2 | ||
| Liver histology | Compatible with AIH | 1 | |
| Typical AIH | 2 | ||
|
YesYes | 2 |
Differential Diagnosis for AIH
The main histologic differential diagnoses for AIH include viral hepatitis, drug/medication-induced liver injury, and primary biliary disorders (primary biliary cholangitis/PBC and primary sclerosing cholangitis/PSC). Narrowing down the differential requires correlation with clinical and serologic findings. Viral hepatitis can be confirmed with positive viral serologies. Drug-induced liver injury (DILI) can be caused by numerous medications. DILI can be suspected if drugs known to cause liver injury are on a patient's medication list. Primary biliary disorders can have florid portal inflammation , mimicking chronic hepatitis injury pattern, but they usually show a cholestatic pattern of injury (elevations of ALP and total bilirubin) and may show more specific serologies (ex. AMA in PBC). On histology there is bile duct damage or loss, and in some cases, characteristic onion-skin fibrosis (PSC) or florid duct lesions (PBC). Lastly, some liver biopsies may show features of both AIH and a primary biliary disorder. This is known as overlap syndrome and will be discussed further in our future posts.
References
- R. Saxena, Practical Hepatic Pathology: A Diagnostic Approach: Second Edition. 2017.
- Torbenson, Atlas of Liver Pathology: A Pattern-Based Approach. 2020.
- Odze and Goldblum, Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas: Third Edition. 2014.
- Lohse AW, Hennes E. Diagnostic criteria for autoimmune hepatitis. Hepatol Res. 2007 Oct;37 Suppl 3:S509. doi: 10.1111/j.1872-034X.2007.00289.x. PMID: 17931212.
- Hennes EM, Zeniya M, Czaja AJ, Parés A, Dalekos GN, Krawitt EL, Bittencourt PL, Porta G, Boberg KM, Hofer H, Bianchi FB, Shibata M, Schramm C, Eisenmann de Torres B, Galle PR, McFarlane I, Dienes HP, Lohse AW; International Autoimmune Hepatitis Group. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008 Jul;48(1):169-76. doi: 10.1002/hep.22322. PMID: 18537184.