Pathology Pearls: Overlap Syndrome
Brief Case Presentation
A 17-year-old male with no significant past medical history presented with abdominal pain, diarrhea, vomiting, and elevated liver enzymes. His inflammatory markers were raised along with elevated lipase levels. Abdominal ultrasound was normal, but MRCP showed findings consistent with chronic pancreatitis with no significant findings in the biliary tree. His fecal calprotectin was elevated which raised concerns for inflammatory conditions of intestine, including IBD. MRE did not show any evidence of ileitis and colitis. Upper endoscopy and colonoscopy were performed with histopathology showing active esophagitis, duodenitis, terminal ileitis, and colitis. There was no evidence of glandular architectural distortion or granulomas. Paneth cell metaplasia was noted in the descending colon. A liver biopsy was subsequently performed.
Selected lab values are as follows:
Liver biopsy findings
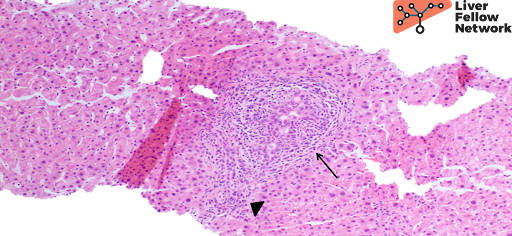
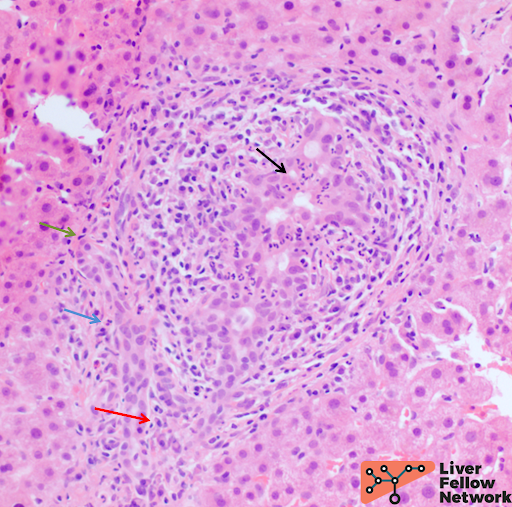
At low power, the liver core shows portal mixed inflammatory infiltrate (Figures 1 and 2).

At high power, acute cholangitis and pericholangitis is seen with focal interface mixed inflammation and prominent plasma cell component (Figure 3).
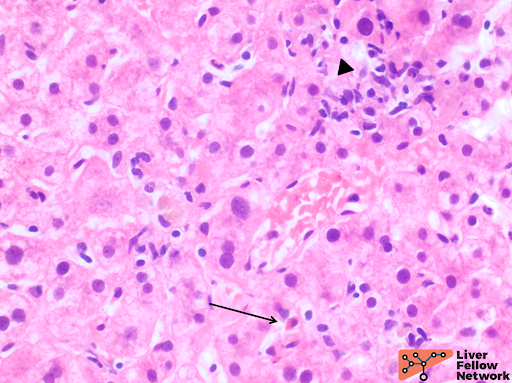
Also seen at high power is mild lobular inflammation (Figure 4).
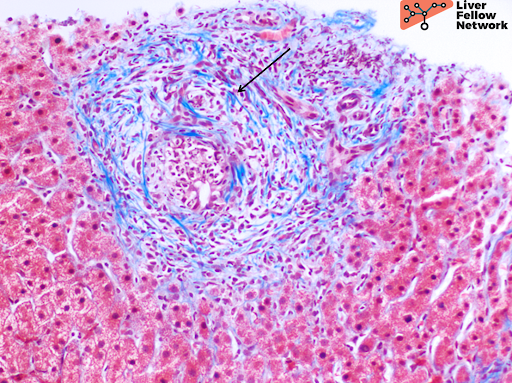
A trichrome stain highlights mild portal fibrosis with focal concentric (“onion skin”) pattern and delicate periportal extensions (Figure 5).
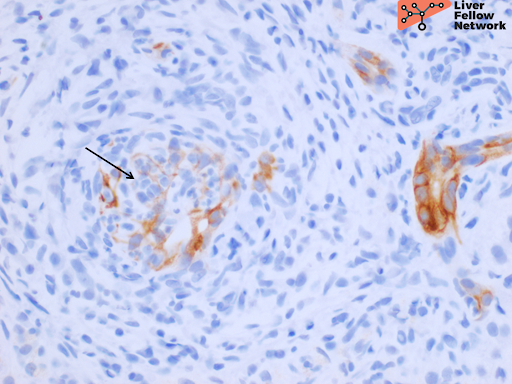
An immunohistochemical stain for CK7 demonstrates the bile duct injury (Figure 6).
In the clinical context provided, the histologic findings are compatible with a primary biliary process most suggestive of primary sclerosing cholangitis and the interface hepatitis, prominent plasma cell infiltrate, and mild lobular inflammation are consistent with an evolving overlap autoimmune hepatitis.
Overview of Overlap Syndromes
Τhe most common overlap syndromes are between primary biliary cholangitis (PBC) and autoimmune hepatitis (AIH) or primary sclerosing cholangitis (PSC) and AIH. PBC and PSC overlap is exceedingly rare. The overall incidence of overlap syndrome ranges between 1%-5%; with one disease process biochemically, clinically, and histologically predominating the other, similar to our case. True incidence of two co-occurring diseases is less than 1%.
Autoimmune sclerosing cholangitis (AIH-PSC overlap)
AIH-PSC overlap is most commonly identified in children with laboratory studies demonstrating a hepatitic pattern of injury in the setting of ulcerative colitis (less commonly Crohn’s disease). For this reason, children presenting with this picture should undergo evaluation of the biliary tree as well as the colon. AIH-PSC overlap has been termed as autoimmune sclerosing cholangitis in the past but due to the confusion with autoimmune cholangitis (without “sclerosing”) (AMA-negative PBC), it is not a preferred term anymore.
AIH-PSC overlap is considered in the setting of bile duct injury or bile ductular proliferation that is more prominent than that seen in cases of AIH alone (positive ANA, ASMA, serum IgG, and inflammatory markers along with biopsy findings of interface hepatitis with plasma cells). Additionally, an ALP higher than 2 times normal is a good check of a primary biliary process seen on histology. It is however, important to remember that ALP and GGT might be mildly increased during the initial stages. A subsequent imaging of the extrahepatic biliary tree is recommended to identify PSC.
Differential Diagnosis for AIH-PSC overlap syndrome
Because AIH-PSC overlap syndrome often presents with predominant findings of one diagnosis, the top differential diagnostic considerations include primary biliary processes alone such as PBC or PSC or an overlap of both or overlap with AIH.
Other differential diagnoses of consideration include IgG4 sclerosing cholangitis, secondary sclerosing cholangitis following biliary surgery, cholelithiasis, congenital biliary abnormalities, ischemic cholangiopathy, infectious cholangiopathy and sclerosing cholangiocarcinoma all of which should be excluded before a diagnosis of PSC or overlap is rendered.
Small duct PSC is another differential that can be considered in the setting of PSC findings on biopsy but a normal cholangiogram since a subset of these cases also show overlap with AIH.
References
Torbenson, Atlas of Liver Pathology: A Pattern-Based Approach. 2019
Torbenson, Surgical Pathology of the Liver. 2018.
Burt, MacSween’s Pathology of the Liver: Seventh Edition. 2017.
Odze and Goldblum, Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas: Third Edition. 2014
