Pathology Pearls Post 8: Primary Sclerosing Cholangitis (PSC)
Brief Case Presentation
A 45-year-old male with a history of inflammatory bowel disease presents with fatigue and right upper quadrant pain. Physical exam is unremarkable. Results from his liver function tests and serologic studies are seen below:
| Lab Value | Result |
|---|---|
| AST | 70 U/L (10-50 U/L) |
| ALT | 90 U/L (10-50 U/L) |
| ALP | 247 U/L (35-130 U/L) |
| Total Bilirubin | 3.3 mg/dL (0.0 – 1.0 mg/dL) |
| HAV | Negative |
| HBV | Negative |
| HCV | Negative |
| ANA | Positive |
| Mitochondrial M2 Ab | Negative |
| Smooth Muscle Ab | Negative |
| IgG | 1700 mg/dL |
Liver Biopsy
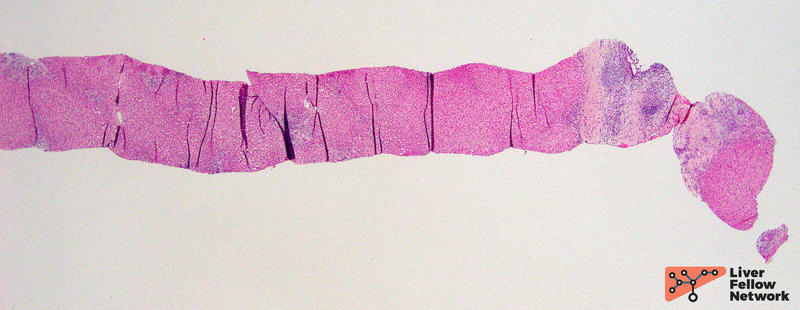
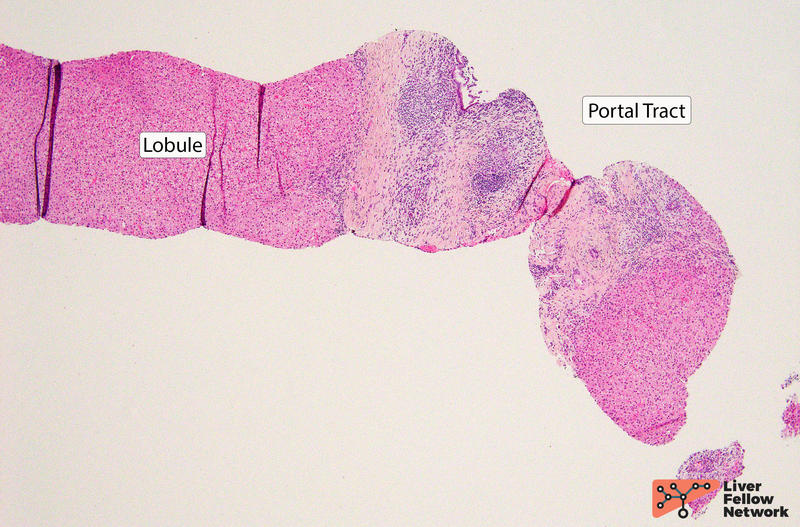
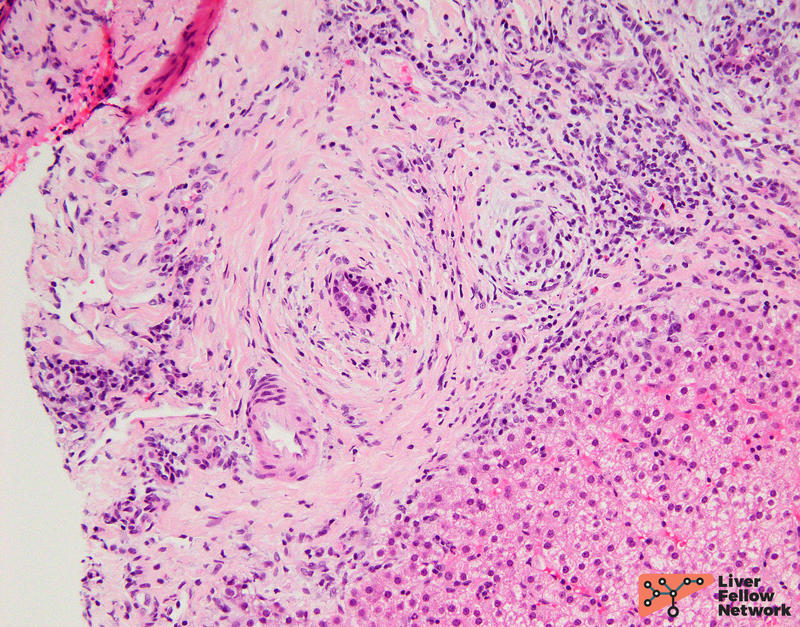
At low and medium magnification, the liver biopsy shows predominantly portal-based changes including inflammation and fibrosis, and minimal to absent lobular activity (Figure 1).
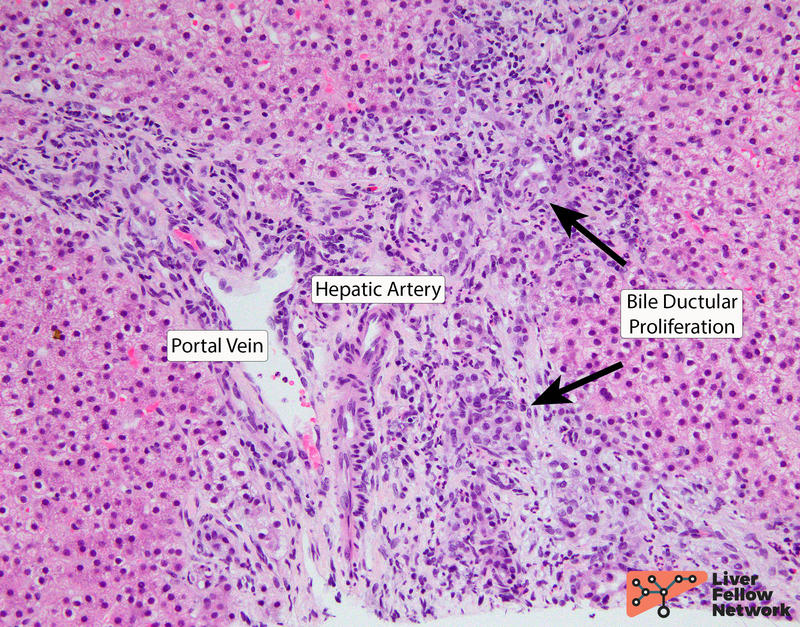
Some portal tracts demonstrate a bile ductular proliferation (Figure 2).
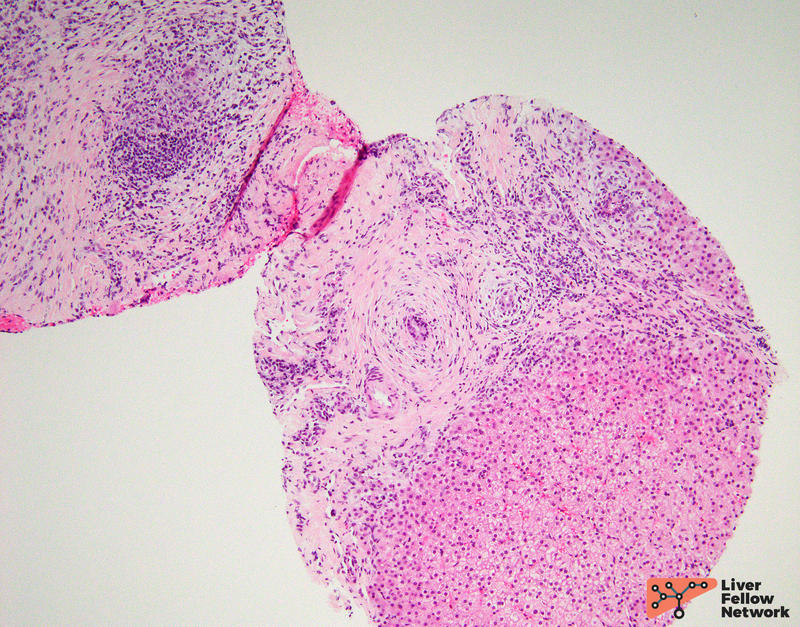
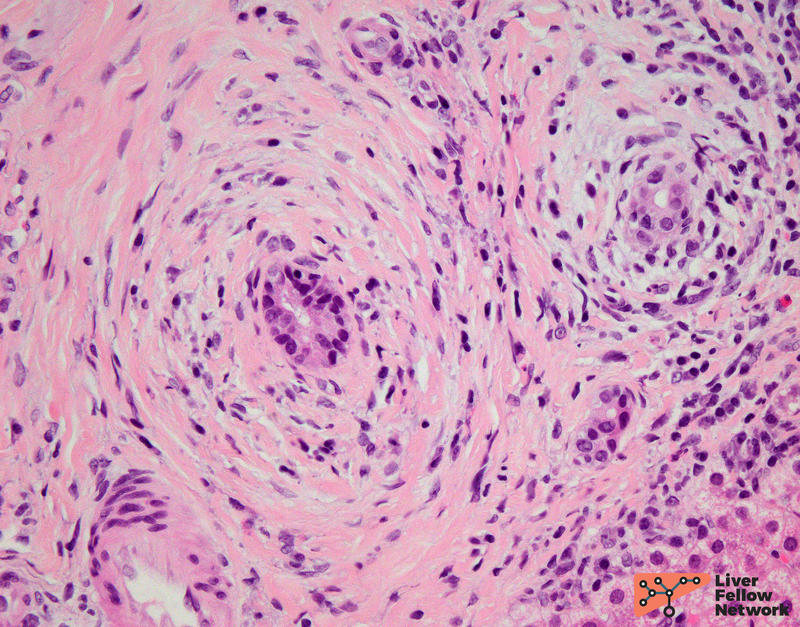
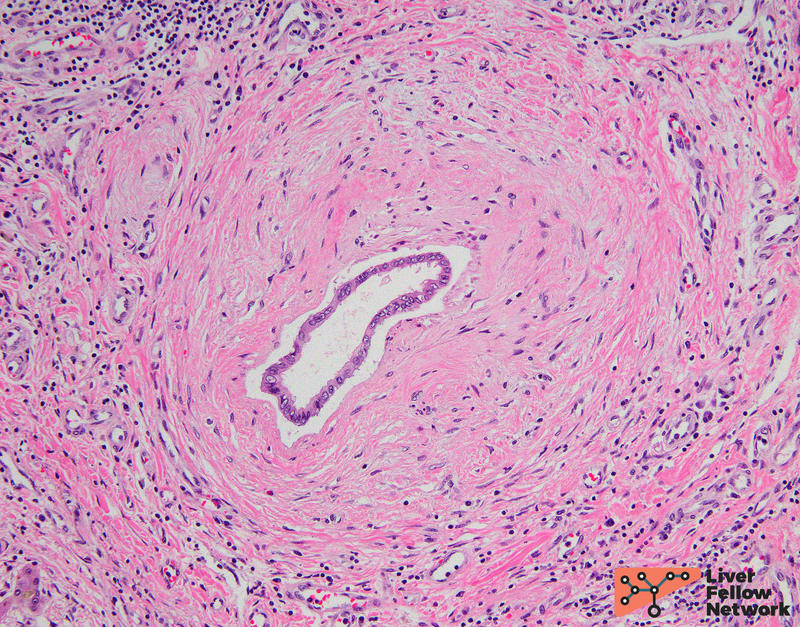
One portal tract reveals bile ducts surrounded by concentric fibrosis (Figure 3).
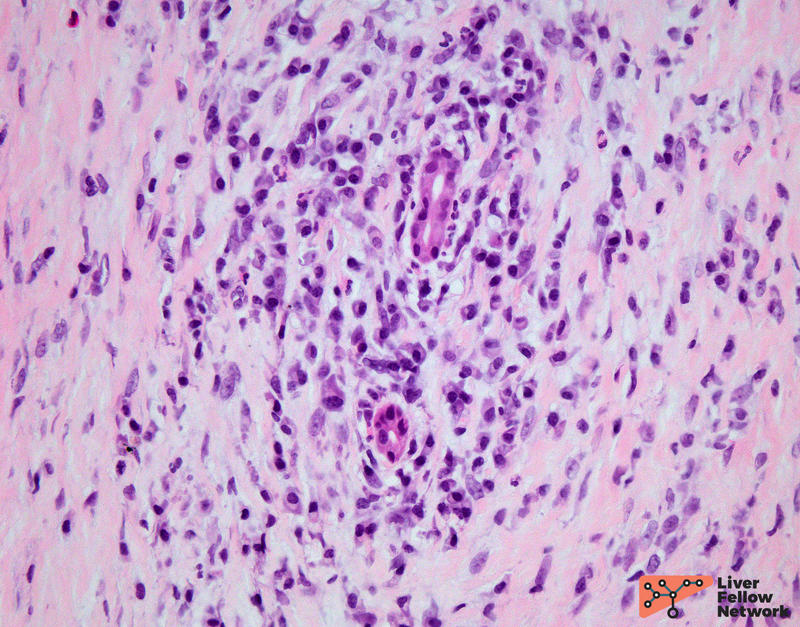
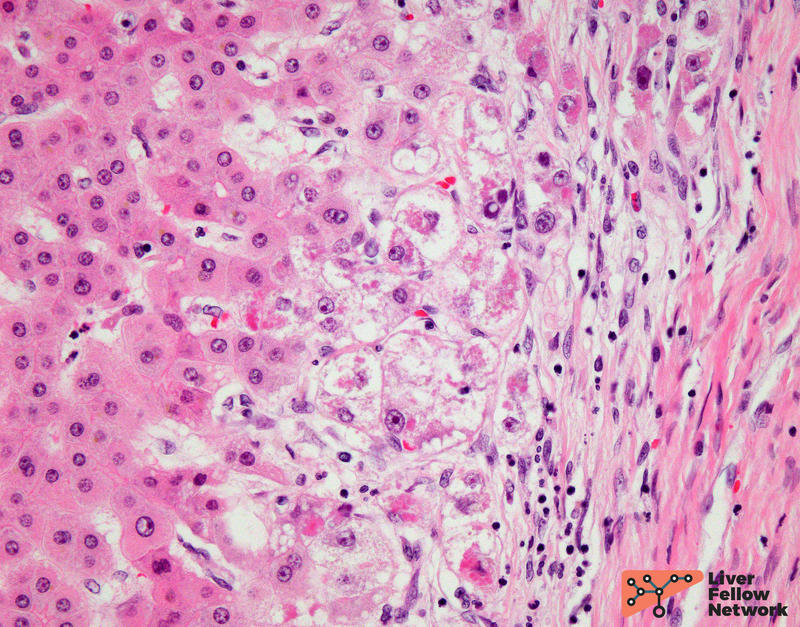
In this biopsy, bile duct injury is seen as nuclear disarray (Figure 4) and cytoplasmic eosinophilia (Figure 5).
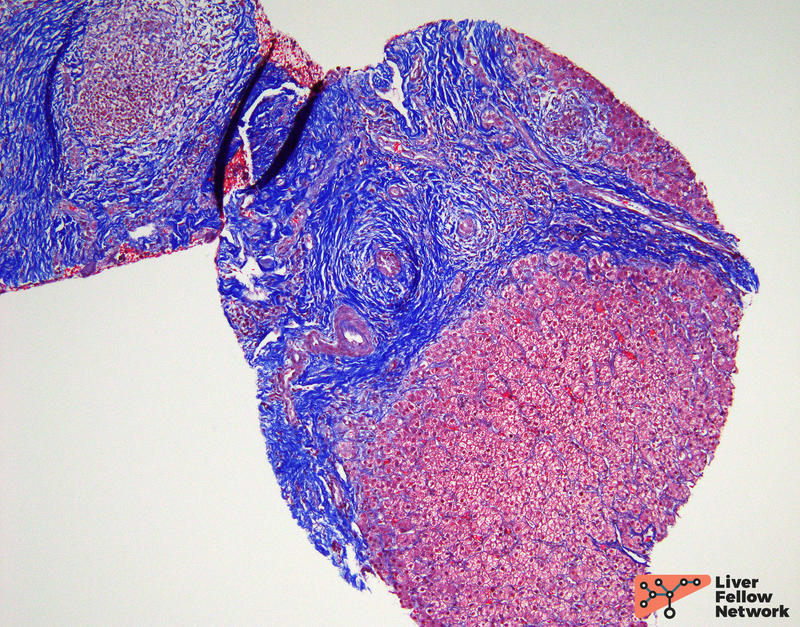
A trichrome stain highlights increased portal fibrosis (Figure 6).
Given the absence of etiology for secondary cholangitis such as infection and neoplasia, the histologic findings are suggestive of primary sclerosing cholangitis (PSC).
Histologic Features of PSC
Although the gold standard for the diagnosis of PSC remains endoscopic retrograde cholangiopancreatography (ERCP) / magnetic resonance cholangiopancreatography (MRCP), a liver biopsy can aid in the diagnosis. Most cases of PSC involve the large intrahepatic and/or extrahepatic bile ducts, which results in a “beads on a string” appearance on ERCP/MRCP. In a smaller percentage of cases PSC involves only the small ducts, thus these changes are often not reflected on imaging.
The most classic findings of PSC include large bile ducts surrounded by concentric fibrosis, which is also referred to as “onion skin” fibrosis (Figure 7).
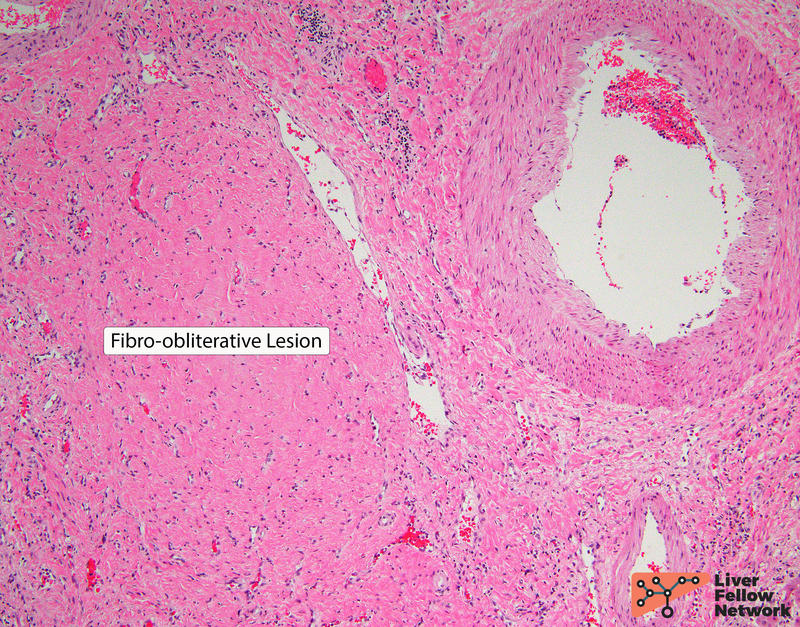
As the disease progresses there is bile duct loss (ductopenia) and fibro-obliterative lesions or scars replace the bile ducts in portal tracts (Figure 8).
When affected large bile ducts are not sampled, findings in liver biopsies from patients with PSC may be nonspecific and can demonstrate portal tracts with increased inflammation and fibrosis. There is usually mild lymphocytic portal inflammation with occasional eosinophils. Neutrophils and plasma cells may also be seen. Bile duct injury may be present; however, the severity depends upon disease duration. Examples of bile duct injury include cytoplasmic vacuolization, epithelial attenuation, and nuclear disarray. Increased intraepithelial lymphocytes may also be identified. Further, secondary changes due to bile duct obstruction may be seen including cholate stasis (Figure 9), bile ductular proliferation, and periportal copper deposition. Over time, chronic injury may result in biliary type cirrhosis – typically described as a “jigsaw puzzle” pattern. There is no to minimal lobular activity.
Differential Diagnoses for PSC
The list of secondary causes of extrahepatic biliary obstruction that can mimic PSC microscopically includes (but is not limited to) gallstones, stricture, tumor, infection, ischemia, irradiation etc. Histologically, biliary obstruction shows mixed portal inflammation (often with increased neutrophils), ductular proliferation, and edema. Canalicular cholestasis can also be seen. The cause of the obstruction is diagnosed utilizing clinical investigations.
Primary biliary cholangitis (PBC) should also be considered in the differential diagnosis of PSC. Liver biopsies of PBC show portal-based inflammation with bile duct injury (see LFN Post 7). In some cases, a florid duct lesion characterized by a granulomatous response is seen. In contrast to PSC, fibro-obliterative scars are not present.
Although less common, IgG4-associated cholangitis can mimic PSC. Liver biopsies with IgG4-associated cholangitis demonstrate portal-based inflammation and periductal fibrosis, but in contrast to PSC there is a greater number of plasma cells, thus the infiltrate is characterized as lymphoplasmacytic. In these cases, immunohistochemistry for IgG4 highlights numerous plasma cells.
References
- R. Saxena, Practical Hepatic Pathology: A Diagnostic Approach: Second Edition. 2017.
- Torbenson, Atlas of Liver Pathology: A Pattern-Based Approach. 2020.
- Odze and Goldblum, Surgical Pathology of the GI Tract, Liver, Biliary Tract and Pancreas: Third Edition. 2014.