Why do patients develop ascites after liver transplantation?
Ascites is a common complication of cirrhosis secondary to hemodynamic changes that cause systemic and splenic vasodilation as result of increased nitric oxide. The presence of ascites is associated with poor survival and liver transplantation is frequently the best treatment option. In this Why series we will discuss ascites in patients after undergoing liver transplantation.
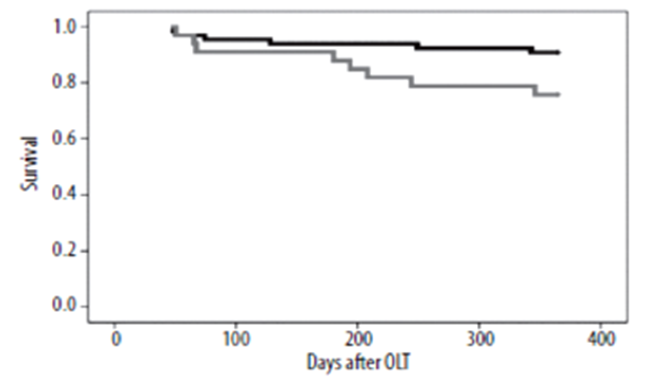
Post-transplant ascites is defined as ascites lasting more than 4 weeks after liver transplantation. Prior data has reported that around 5-7% of patients will develop significant post-transplant ascites and this is supported by a recent retrospective study reporting that 6.3% of patients developed significant ascites after liver transplantation. Although refractory post-transplant ascites is rare, it is associated with high morbidity and mortality. Treatment of refractory ascites includes medications but often requires invasive procedures including paracentesis, TIPS, splenic artery embolization and/or splenectomy. More importantly, refractory post-transplant ascites is associated with a reduced 1-year survival.
Gotthardt DN, Weiss KH, Rathenberg V, Schemmer P, Stremmel W, Sauer P. Persistent ascites after liver transplantation: etiology, treatment and impact on survival.
Ann Transplant. 2013 Jul 24;18:378-83. Doi: 10.12659/AOT.883982. PMID: 23881303.
Etiology
Proposed mechanisms for development of post-transplant ascites include vascular, hepatic, and extrahepatic etiologies. However, up to one third of patients with refractory ascites have no clear etiology of ascites despite undergoing extensive evaluation.
Vascular
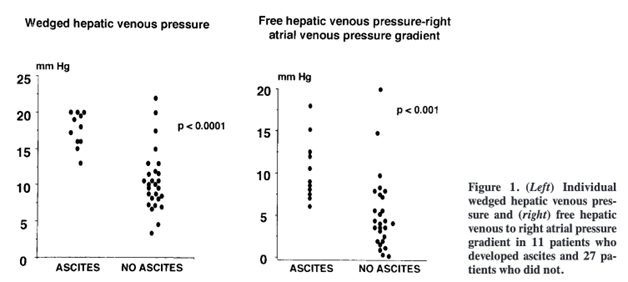
One of the most common causes of persistent post-liver transplant ascites is hepatic outflow obstruction. Cicera et al, found that that the gradient between free hepatic vein and right atrial pressures was significantly greater in patients who developed ascites than in patients who did not. However, ascites only appeared when the wedged hepatic venous pressure, which mirrors sinusoidal pressure, reaches a threshold value of 12 mmHg.
Cirera, I., Navasa, M., Rimola, A., García-Pagán, J.C., Grande, L., Garcia-Valdecasas, J.C., Fuster, J., Bosch, J. and Rodes, J. (2000), Ascites after liver transplantation. Liver Transpl, 6: 157-162.
Hepatic outflow obstruction is caused by stenosis of the caval anastomosis. Incidence is 1% and it can occur regardless of the surgical technique used, including piggyback or caval anastomosis. A recent study showed that up to 17% of patients with post-transplant ascites underwent hepatic vein intervention due to hepatic venous outflow obstruction.
Portal vein thrombosis is a rare cause of post-transplant ascites, and it is thought to be related to vessel reconstruction. The incidence is 1-2% and it is more common in patients with prior history of portal vein thrombosis. Other rare vascular causes of post-transplant ascites include portal vein stenosis and arterioportal fistulas.
Hepatic
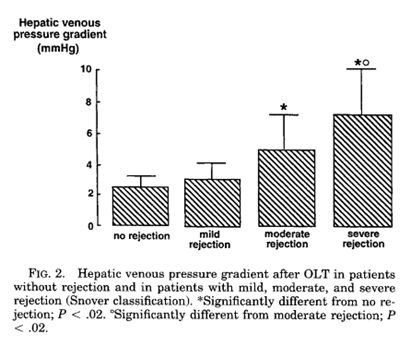
Severe acute cellular rejection (ACR) after liver transplantation has been reported as a cause of post-transplant ascites. It has been proposed to be due to a high hepatic venous pressure gradient (HBPG), with significantly higher HBPG in severe ACR compared to moderate, mild and patients without ACR. There was resolution of ascites after treatment of ACR.
Gadano, A., Hadengue, A., Widmann, J.J., Vachiery, F., Moreau, R., Yang, S., Soupison, T., Sogni, P., Degott, C., Durand, F., Bernuau, J., Belghiti, J., Erlinger, S., Benhamou, J.P. and Lebrec, D. (1995), Hemodynamics after orthotopic liver transplantation: Study of associated factors and long-term effects. Hepatology, 22: 458-465.
Studies have shown that prolonged cold ischemic (CI) time can cause post-transplant ascites by damaging sinusoidal endothelium that leads to decreased production of nitric oxide, resulting in increased vasoconstriction and elevated portal pressure.
Predictors of post-transplant ascites
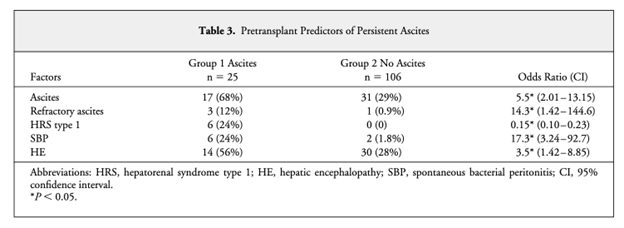
Possible predictors for post-transplant ascites include prior ascites, refractory ascites, hepato-renal syndrome AKI, spontaneous bacterial peritonitis, hepatic encephalopathy, and CI time. A retrospective study found that pre-transplant serum creatinine >1.5 mg/dL, more than 1000 mL of ascites at laparotomy, recipient spleen to graft volume ratio > 1.3, left lobe graft and graft recipient weight ratio < 0.8 were risk factors for recurrent post-transplant ascites.
Stewart CA, Wertheim J, Olthoff K, Furth EE, Brensinger C, Markman J, Shaked A. Ascites after liver transplantation--a mystery. Liver Transpl. 2004 May;10(5):654-60. doi: 10.1002/lt.20106. PMID: 15108257.
Extrahepatic
Non-hepatic causes of ascites post-transplant should be considered. Etiologies including heart failure, end stage renal disease, malignancy, and protein-losing enteropathy should be evaluated in cases of post-transplant ascites.
Evaluation
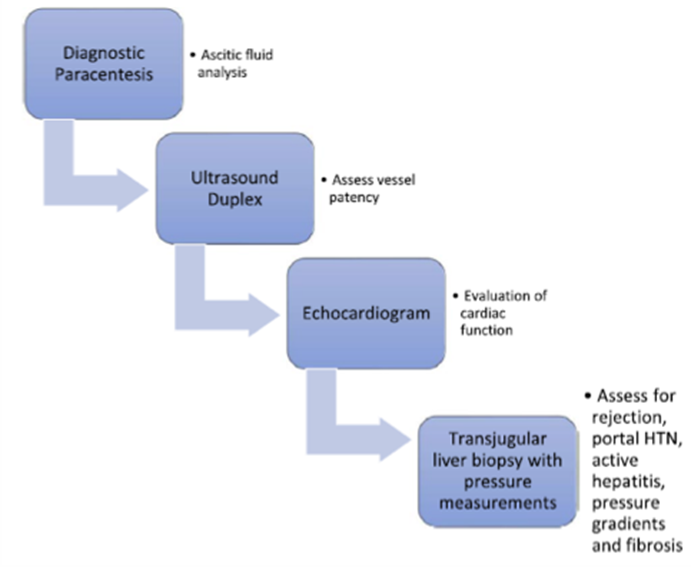
Blood analysis including complete blood cell counts, liver enzymes, albumin level, immunosuppressant level and pro B-type natriuretic peptide should be obtained. The next step in evaluation should be a diagnostic paracentesis with body fluid analysis. However, serum to ascites albumin gradient (SAAG) is not helpful as in the pre-transplant setting. Bloom et al showed that over time, ascites testing including SAAG were performed less often in post-transplant patients with hepatic vein pressure measurements performed with increasing frequency. It also reported that SAAG did not influence subsequent testing, management, or clinical remission at 6 months.
Next step includes ultrasound of the liver with Doppler and/or contrast-enhanced cross-sectional study to evaluate possible vascular etiology as well as measure the liver gradient and spleen size (we will get to why this may matter later in this post). In patients where a cardiac cause is a possibility, transthoracic echocardiogram should be performed. If diagnosis remain unclear, transjugular liver biopsy with pressure measurements and venogram can be considered to evaluate pressure gradients, portal hypertension, and presence of active hepatitis or fibrosis.
Jenkins M, Satoskar R. Ascites After Liver Transplantation. Clin Liver Dis (Hoboken). 2021 May 1;17(4):317-319. doi: 10.1002/cld.1050. PMID: 33968396; PMCID: PMC8087930.
Treatment
Most patients have clinical resolution of ascites within 6 months with most of them requiring only diuretics and paracentesis. Treatment should also target the underlying cause if identified and modifiable. Patients with hepatic outflow obstruction can undergo balloon angioplasty +/- stent implantation or surgical reconstruction. Patients with ACR should have immunosuppressive therapy modified. Patients with heart failure and end stage renal disease should be evaluated by specialists and undergo treatment per recommendations.
All patients with clinically significant ascites should be treated with diuretics. If large or refractory, the patient should undergo therapeutic paracentesis. In patients with unknown etiology treatment options include transjugular intrahepatic portosystemic shunt (TIPS) and splenic artery embolization. TIPS after liver transplantation has a clinical success between 16 to 57% and graft survival 6 to 12 months after TIPS of 45% to 50%. Possible complications include acute liver failure, renal failure, infection, TIPS dysfunction and hepatic encephalopathy.
Splenic artery embolization has emerged as a possible treatment for post-transplant ascites. Patients with larger spleens (spleen to liver volume ratio is > 0.5) have been noted to show the greatest efficacy from this procedure. It is proposed that occluding the splenic artery and decreasing flow through the spleen and splenic vein leads to decreased portal vein pressure gradients and diminishing portal hypertension. Ultimately, it decreases portal vein velocity, decreases diuretic requirements, and lead to weight loss and resolution of ascites.
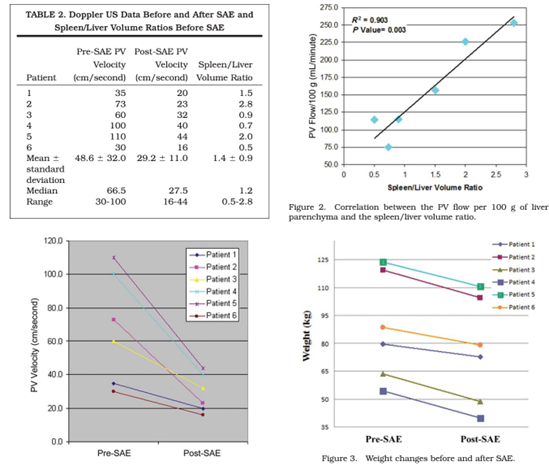
Quintini C, D’Amico G, Brown C, Aucejo F, Hashimoto K, Kelly DM, Eghtesad B, Sands M, Fung JJ, Miller CM. Splenic artery embolization for the treatment of refractory ascites after liver transplantation. Liver Transpl. 2011 Jun;17(6):668-73. Doi: 10.1002/lt.22280. PMID: 21618687
Possible complications from the procedure includes post-embolic syndrome (abdominal pain, nausea, and low-grade fever), spontaneous bacterial peritonitis, high-grade fever, and inferior vena cava thrombus. It has been recommended to perform proximal rather than distal splenic artery embolization, minimizing the risk of complications since it allows distal revascularization.
Vascular etiologies of post-LT ascites can be treated with angioplasty, stent placement, possible surgical revision.
Conclusions
Post-transplant ascites is an uncommon complication but can result in high morbidity and mortality. Possible etiologies include vascular, hepatic, and extrahepatic causes. A significant number of patients with refractory ascites have no clear etiology of ascites identified despite undergoing extensive evaluation. Evaluation includes a stepwise approach that helps guide management. Treatment should be targeted to specific etiology if identified. If etiology is unknown, treatment includes diuretics and paracentesis. In cases of failure to conservative treatment, TIPS can be considered but it is less effective compared to pre-transplant setting. Splenic artery embolization has emerged as an effective and safe treatment option.
Key Points
- Post-transplant ascites is defined as ascites lasting more than 4 weeks after liver transplantation with incidence around 5-7% in patients that undergo liver transplantation.
- Although refractory post-transplant ascites is rare, it is associated with high morbidity and a reduced 1-year survival.
- Post-transplant ascites can result from vascular complications, or hepatic and extrahepatic etiologies. Up to one third of patients have no clear etiology despite undergoing extensive evaluation.
- 72% of patients have clinical resolution of post-transplant ascites within 6 months with some requiring diuretics and paracentesis.
- Treatment of refractory post-transplant ascites includes transjugular intrahepatic portosystemic shunt and splenic artery embolization.
