An Approach to the Cholestatic Infant
An MMP7 level was checked and was elevated at 132.2 (high probability of BA based on internal assay levels).
Additional evaluation included MMP7 as a serum biomarker for biliary atresia in addition to alpha-1-antitrypsin level and phenotype, urine CMV, hepatic function panel and GGT. MMP7 has been shown to be the most specific predictor of biliary atresia other than liver biopsy. However, liver biopsy is still considered the gold standard at this time and should not be delayed for laboratory results from MMP7 due to time-sensitive nature of biliary atresia diagnosis with outcomes inversely proportional to age at time of therapeutic portoenterostomy surgery.
Back to the Basics:
Hyperbilirubinemia:
Hyperbilirubinemia in infancy is defined as serum conjugated/direct bilirubin level >1 mg/dL and > 20% of the total bilirubin.
When to be concerned about an infant with jaundice:
Jaundice at or beyond 2 weeks of age should be evaluated with fractionation of serum bilirubin. With data from the past decade, 1mg/dL conjugated/direct bilirubin should be the threshold to do further evaluation for hepatobiliary causes rather than just 20% of total bilirubin as this has level has been shown in the newborn period to be a specific threshold for biliary atresia patients.
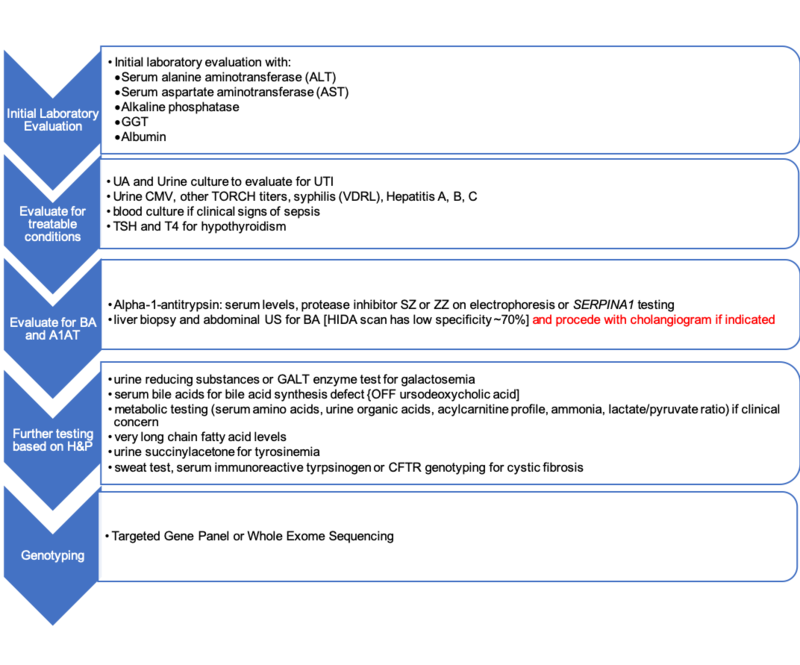
Overview of approach to an infant with cholestasis, evaluate for:
- Anatomic anomalies or evidence of obstruction including biliary atresia (classic but non-diagnostic findings include small or absent gallbladder, triangle cord sign), evidence of biliary atresia with splenic malformation caused by genetic defects (polysplenia, laterality defects), or choledochal cyst with abdominal ultrasound
- Infectious etiology such as UTI, TORCH infection (commonly CMV) or any septicemia
- Genetic or metabolic disorders with hepatic involvement including Alagille’s, alpha-1-antityrpsin deficiency, cystic fibrosis, Dubin-Johnson syndrome, tyrosinemia, bile transporter defects and galactosemia
- Endocrine abnormality including hypothyroidism, panhypopituitarism
- Toxins including drugs, TPN, and some herbal products
- Immune Mediated/Other: HLH/GALD, ischemic/hypoxic/congestive injury, oncologic, idiopathic neonatal hepatitis (INH)
Figure 1: Diagnostic Approach:
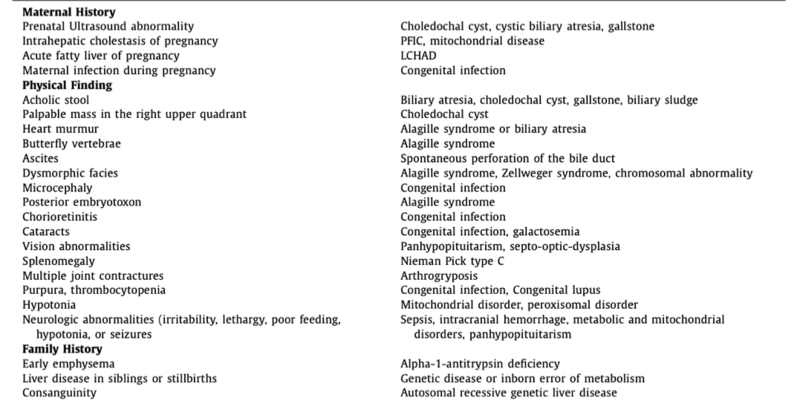
Figure 2: Key points from history or physical and related etiologies of neonatal cholestasis
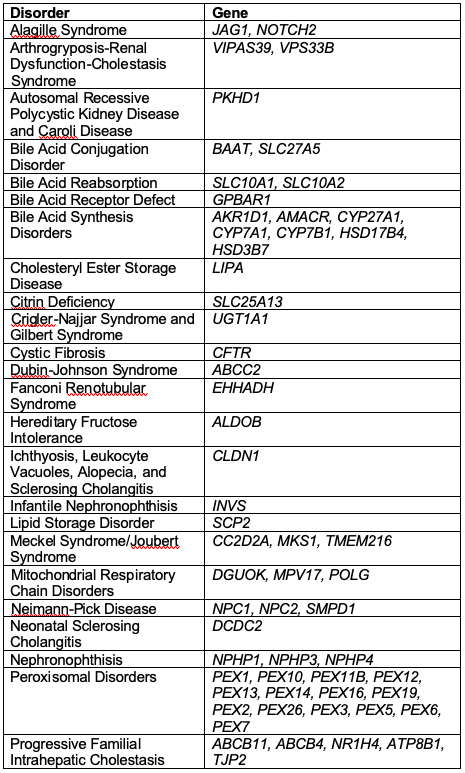
The era of personalized medicine:
It has been discussed that genetic panels may become the new gold standard and may supersede other testing in the near future as these technologies become more efficient and affordable. Currently available testing includes targeted gene panels, whole exome sequencing, or whole genome sequencing
Highlighted manifestations of inherited disorders of cholestasis in adulthood
Recommended reading in Clinical Liver Disease
Figure 3: Genes and Associated Cholestatic Disorders
References:
- Feldman A , Suchy FJ . Approach to the infant with cholestasis. In: Suchy FJ, Sokol RJ, Balistreri WF, eds. Liver Disease in Children. New York City: Cam- bridge University Press; 2014:101–110
- Harpavat S , Finegold MJ , Karpen SJ . Patients with biliary atresia have elevated direct/conjugated bilirubin levels shortly after birth. Pediatrics . 2011;128(6):e1428–e1433
- Jiang J , Wang J , Shen Z , Lu X , Chen G , Huang Y , et al. Serum MMP-7 in the diagnosis of biliary atresia. Pediatrics . 2019;144(5)
- Serinet MO, Wildhaber BE, Broué P, Lachaux A, Sarles J, Jacquemin E, Gauthier F, Chardot C. Impact of age at Kasai operation on its results in late childhood and adolescence: a rational basis for biliary atresia screening. Pediatrics. 2009 May;123(5):1280-6.
- Fawaz R , Baumann U , Ekong U , Fischler B , Hadzic N , Mack CL , et al. Guideline for the evaluation of cholestatic jaundice in infants: joint recommendations of the North American society for pediatric gastroenterology, hepatology, and nutrition and the European society for pediatric gastroenterology, hepatology, and nutrition. J Pediatr Gastroenterol Nutr . 2017;64(1):154–168 .
- De Bruyne R, Van Biervliet S, Vande Velde S, Van Winckel M. Clinical practice: neonatal cholestasis. Eur J Pediatr. 2011 Mar;170(3):279-84
- Brumbaugh D, Mack C. Conjugated hyperbilirubinemia in children. Pediatr Rev. 2012 Jul;33(7):291-302.
- Suchy FJ . Neonatal cholestasis. Pediatr Rev . 2004;25(11):388–396 .
- Goldberg A, Mack CL. Inherited Cholestatic Diseases in the Era of Personalized Medicine. Clin Liver Dis (Hoboken). 2020 Apr 4;15(3):105-109.