Peeling Back The Layers of Pediatric Primary Sclerosing Cholangitis
Pathophysiology and Natural History
Primary sclerosing cholangitis (PSC) is a chronic, cholestatic liver disease, thought to be immune-mediated in nature, characterized by inflammation and fibrosis of extrahepatic and intrahepatic bile ducts. Some processes that have been proposed to play a role in the pathogenesis of PSC include bile acid toxicity, diminished biliary bicarbonate umbrella, aberrant lymphocyte homing, leaky gut, and intestinal dysbiosis. PSC leads to cirrhosis, portal hypertension, and hepatic decompensation in the majority of patients. It is estimated that about 30% of children will require a liver transplant within 10 years of diagnosis of PSC.
Incidence and Prevalence
PSC is rare in the general pediatric population, with an estimated incidence and prevalence of 0.2 and 1.5 cases per 100,000 children, respectively. PSC affects at least 10% of children with ulcerative colitis (UC), and it is estimated that around 76% of children with PSC have concomitant inflammatory bowel disease (IBD).
Definitions
PSC overlap syndromes are conditions with diagnostic features of both PSC and other immune-mediated liver diseases such as autoimmune hepatitis (AIH), commonly called PSC/AIH overlap or autoimmune sclerosing cholangitis, autoimmune pancreatitis, and rarely in adults primary biliary cirrhosis (PBC). Large duct PSC is defined as disease that is noted on imaging studies. In contrast, small duct PSC is a disease variant which is characterized by typical cholestatic and histological features of PSC but normal bile ducts on cholangiography.
Differences between Adult and Pediatric PSC
Though the pathogenesis of PSC is elusive, it is possible that driving factors such as the interaction between genetics, the environment, and the microbiome may be skewed differently in children compared to adults, thereby leading to disease development at a younger age, similar to IBD.At diagnosis, dominant strictures are typically present in as many as 45% of adults but only about 4% of children. The incidence of small duct PSC is higher in children (~20%) than adults (<5%). Children also more often have features of PSC/AIH overlap (>33%) compared to adults (7%). Alkaline phosphatase (ALK-P), which is a key marker of cholestatic liver disease in adults, is not as reliable in children as it can be elevated from higher bone turnover in growing children. Instead, GGT is more commonly used as a biomarker in both clinical and research practices in pediatric patients with PSC. Additionally, children often do not have other risk factors for progression of liver disease, such as alcohol abuse and polypharmacy. Therefore, pediatric PSC may be a different disease process compared to adult PSC.
Diagnosis
The diagnosis of PSC is made in patients with labs demonstrating cholestasis, cholangiography showing characteristic bile duct changes with multifocal strictures and segmental dilations of the intrahepatic and extrahepatic bile ducts, and exclusion of secondary causes of sclerosing cholangitis.
Elevations in AST, ALT, GGT, and ALK-P will often be noted in pediatric patients with PSC. Most patients will undergo right upper quadrant ultrasound first to exclude biliary obstruction. If obstruction is not found, then cholangiography is the next step. MRCP is the preferred modality given that it is non-invasive, less expensive, and has no risk of associated pancreatitis compared to endoscopic retrograde cholangiopancreatography (ERCP). However, ERCP allows direct visualization of the bile ducts and can be utilized for therapeutic interventions such as tissue sampling, removal of mechanical obstructions such as stones, and dilation of symptomatic or dominant strictures.
Given that many patients with PSC have concomitant IBD, screening esophagogastroduodenoscopy and colonoscopy with biopsies is often recommended.
Given the high incidence of PSC/AIH overlap in pediatrics, AASLD guidelines recommend that all pediatric patients with PSC undergo liver biopsy to evaluate for evidence of AIH. Additionally, total IgG, ANA, anti-smooth muscle antibody and anti-LKM antibody should be sent. Histologic findings consistent with PSC/AIH overlap can include periductal concentric fibrosis, portal and interface mixed inflammation, and plasma cell infiltrate (check out an awesome LFN Pathology Pearls about overlap syndrome). Liver biopsy should also be performed to evaluate for small duct PSC in the setting of normal cholangiography but labs consistent with PSC.
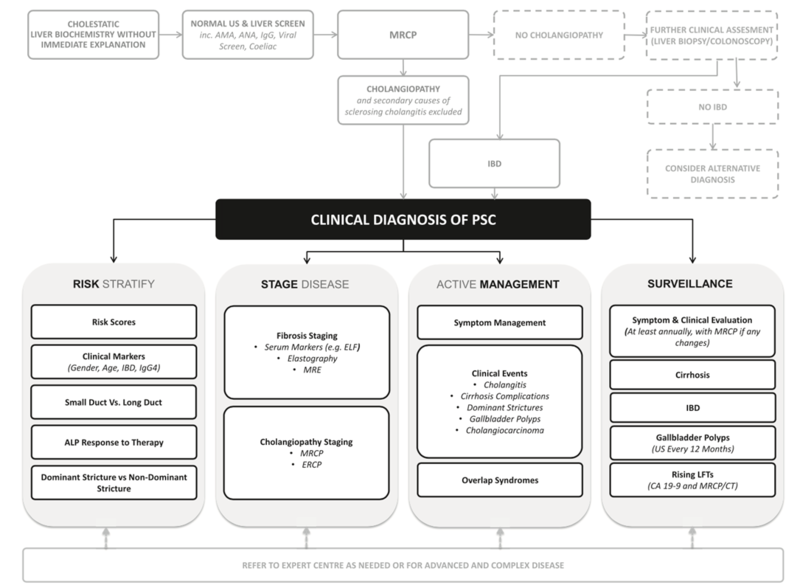
Diagnostic Algorithm
Taken from: Lindor KD, Kowdley KV, and Harrison ME. ACG Clinical Guideline. Am J Gastroenterol. 2015;110(5): 646-59.
Treatment
Ursodeoxycholic acid (UDCA) is the best studied treatment in adult patients with PSC. A previous randomized controlled trial of patients receiving UDCA at 13-15 mg/kg/day demonstrated biochemical improvement that did not reach statistical significance. Another study testing higher doses of UDCA up to 20 mg/kg/day showed the drug was well tolerated but did not significantly impact long term outcomes. A large Swedish randomized trial tested doses of UDCA (17-23 mg/kg/day), however this study was underpowered and did not show significant differences in rates of death, transplantation, or development of cholangiocarcinoma. At the same time a large double blind, randomized controlled trial using UDCA at 28-30 mg/kg/day compared to placebo was conducted by Lindor et al, but had to be terminated early due to futility with biochemical improvements and an increased risk of death, transplant, meeting minimal listing criteria, development of varices, cholangiocarcinoma or progression to cirrhosis in the UDCA treatment group. Therefore, AASLD guidelines currently recommend against the use of UDCA in the treatment of adult PSC.
Given that there are many differences between adult and pediatric PSC, there are no firm guidelines against the use of UDCA in children. It is a well-tolerated medication at doses of 15-20 mg/kg/day. It does seem to be associated with significant biochemical improvements, but its long-term benefits are still unclear. Moreover in studies of UDCA compared to placebo, many patients who did not receive therapy still had biochemical improvements in their GGT demonstrating that patients with PSC may have normalization of their liver enzymes without treatment.
Treatment with corticosteroids and other immunosuppressant agents have not demonstrated any improvement in disease activity or in the outcome of PSC. However, these drugs may well have a role in the context of a PSC/AIH overlap syndrome, as pediatric patients with evidence of PSC/AIH overlap syndrome are more likely to respond to immunosuppressive treatment such as azathioprine.
Oral vancomycin has anecdotally shown some benefit in clinical symptoms and liver biochemistries in some patients, particularly in the pediatric age group. No formal randomized controlled trials have been conducted to test this medication yet.However, Deneau et al conducted a propensity-score patient-matched study comparing oral vancomycin, UDCA, and no treatment. This study found that there was no difference in biochemical response, fibrosis score, or long term outcomes such as probability of liver transplant listing between the three groups, suggesting that neither UDCA nor oral vancomycin were superior to the other, and pediatric patients with PSC may experience spontaneous biochemical normalization even without treatment.
Liver transplantation is indicated in patients with complications of portal hypertension and end stage liver disease.
Prognosis Index
The Sclerosing Cholangitis Outcomes in Pediatrics (SCOPE) Index is a pediatric-specific prognostic tool for PSC that correlates strongly with fibrosis on liver biopsy. The SCOPE index will be discussed in greater detail in a future Evidence Corner post on the Liver Fellow Network blog. Stay tuned!