Biliary Ductal Dilation: Just Another Case of Malignancy?
Epidemiology and Presentation of IgG4 Cholangiopathy
IgG4 cholangiopathy is an autoimmune disorder that manifests as inflammation of the bile ducts, which can progress to ductopenia, cirrhosis, and bile duct cancer. This disease is often accompanied by IgG4 related diseases affecting other organs, including the lacrimal and salivary glands and most commonly the pancreas. Unlike many other autoimmune disorders, there is a male predominance, with a 3.3:1 male to female ratio. The age at diagnosis varies, between 14-85, however the average age at diagnosis is 69.
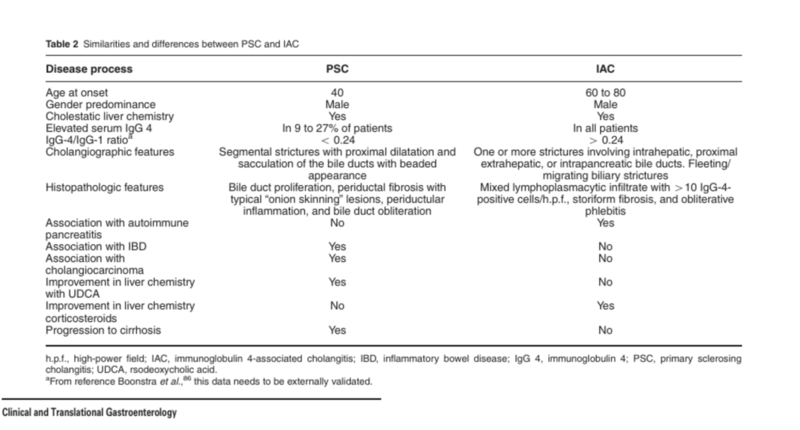
The presentation of IgG4 cholangiopathy is highly variable. The most common presenting sign is jaundice, with an estimated 77% of patients developing it prior to evaluation. Other common symptoms include weight loss and abdominal pain, and new onset diabetes has also been reported. IgG4 cholangiopathy should always be considered as a possible diagnosis when evaluating a patient for primary sclerosing cholangitis (PSC), although it has been reported that approximately 9% of patients with PSC have high serum IgG4 levels in the absence of IgG4 cholangiopathy. Important clinical distinctions between IgG4 cholangiopathy and PSC are noted in Table 1.
Table 1 - Clinical distinctions between IgG4 cholangiopathy and primary sclerosing cholangitis
Current Concepts in Primary Biliary Cirrhosis and Primary Sclerosing Cholangitis. Clin Transl Gastroenterol 2015. IAC is another term for IgG4 cholangiopathy.
Diagnosis of IgG4 Cholangiopathy
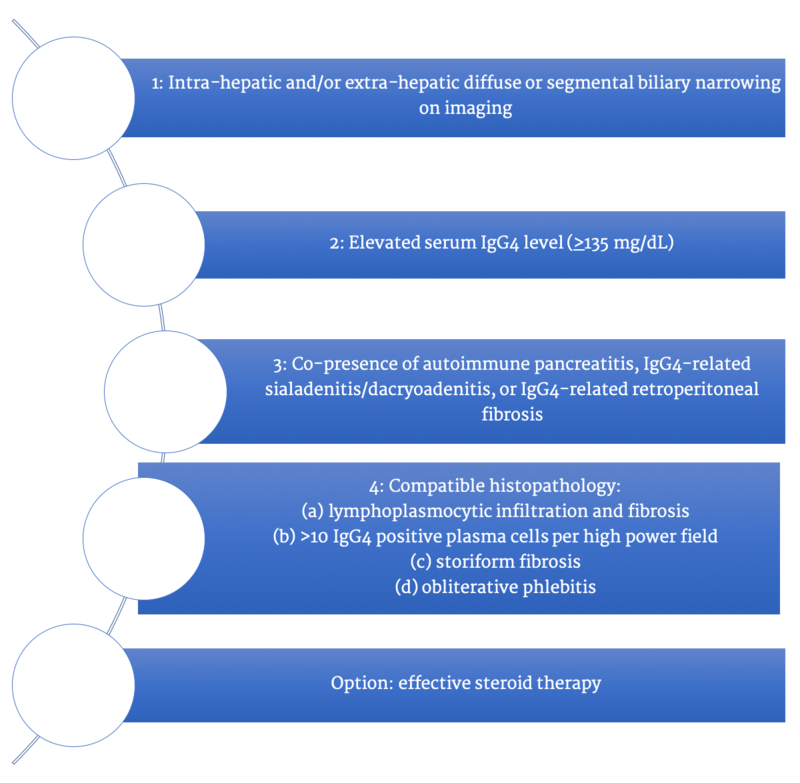
Making a diagnosis of IgG4 cholangiopathy is challenging. Contrary to the name of this condition, approximately 10% of patients with IgG4 cholangiopathy do not have elevated levels of serum IgG4. The Japan Biliary Association has proposed standardized diagnostic criteria for IgG4 cholangiopathy as shown in Figure 1.
Figure 1 - Proposed diagnostic criteria by the Japan Biliary Association
Taken from: Clinical Diagnostic Criteria of IgG4-related Sclerosing Cholangitis. J Hepatobiliary Pancreat Sci 2012.
A definitive diagnosis is made with options 1 and 3; 1, 2, and 4 (a and b); 4 (a, b, and c); and 4 (a, b, and d).
Figure 2 - Example of obliterative phlebitis (destruction of small veins due to lymphoplasmacytic infiltration and ultimately fibrosis) on histopathology
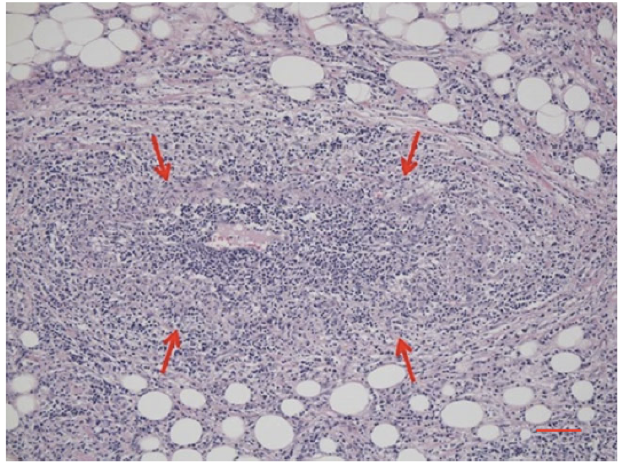
Taken from: Clinical Practice Guidelines for IgG4-related sclerosing cholangitis. J Hepatobiliary Pancreat Sci 2019.
Treatment for IgG4 Cholangiopathy
The mainstay of treatment for IgG4 cholangiopathy is steroids. Guidelines recommend initiating prednisolone at 0.6mg/kg/day for induction, with a goal to reduce the dose of prednisolone to 5mg/day within three months. This dose should be maintained for a minimum of three years, with serial clinical, laboratory, and radiologic monitoring.
Figure 3- Guidelines for treating IgG4 cholangiopathy
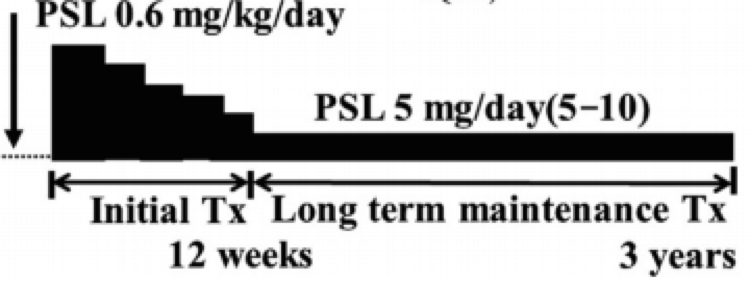
Taken from: Clinical Diagnostic Criteria of IgG4-related Sclerosing Cholangitis. J Hepatobiliary Pancreat Sci 2012.