Management of Refractory Ascites in Cirrhosis
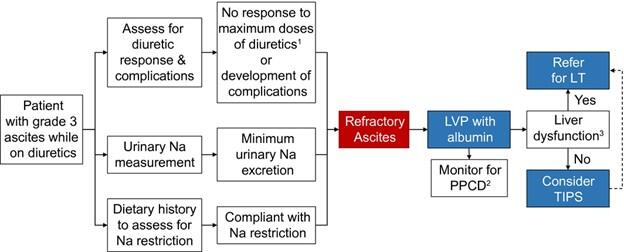
This patient has diuretic-resistant ascites, also referred to as refractory ascites. Survival in patients with refractory ascites is 50% at 6 months and 25% at 1 year.
Refractory ascites in patients with cirrhosis is present if at least one of the following criteria is present in the absence of nephrotoxic medications:
- Inability to mobilize ascites despite adherence to dietary sodium restriction of 2 g per day and maximum tolerable doses of oral diuretics (spironolactone 400 mg/day and furosemide 160 mg/day; the caveat is that these doses are rarely reached due to adverse reactions); diuretic resistant ascites
- Rapid reaccumulation of fluid after therapeutic paracentesis despite dietary sodium restriction
- The development of diuretic-related complications such as progressive azotemia, hepatic encephalopathy, or progressive electrolyte imbalance; diuretic intractable ascites
1. Rule out other entities that lead to refractory ascites
- Malignant ascites, Budd-Chiari syndrome, portal vein occlusion, chylous ascites, and nephrogenic ascites
- Perform diagnostic paracentesis and abdominal ultrasound with Doppler imaging
- Discontinue medications that decrease systemic blood pressure, non-steroidal anti-inflammatory drugs (NSAIDs)
- Consider starting midodrine (start at 5 mg orally three times a day and adjust the dose in increments of 2.5 mg with each dose to a maximal dose of 17.5 mg orally three times a day) to achieve a mean arterial pressure of > 82 mmHg
- Continue dietary sodium restriction.
2. What if initial treatment fails?
- Referral to a liver transplantation center if not already listed. However, for patients whose major complications of liver cirrhosis are related to portal hypertension alone, like refractory ascites, MELD score does not always reflect the effect this complication has on their quality of life. Priority for liver transplantation (LT) remains low, as no exception points can be gained for this condition at this time.
- Serial large-volume paracentesis (LVPs; arbitrarily defined as a paracentesis of > 5 L) with albumin to prevent post paracentesis circulatory dysfunction (PPCD; 6-8 g of albumin per liter of ascites removed). There is evidence showing inferior survival with LVPs when compared to TIPS in selected patients.
- TIPS is recommended by the American Association for the Study of Liver Diseases (AASLD) for patients who are intolerant of repeated large volume paracentesis. When starting an evaluation for TIPS, keep the following relative contraindications in mind: severe hepatic dysfunction (Child-Pugh Class C cirrhosis, MELD Score 18+), age over 65 years, lack of support in the home to monitor post-TIPS complications, active alcohol associated hepatitis, cardiac ejection fraction < 60%, pulmonary hypertension, or history of hepatic encephalopathy.
- Permanent indwelling peritoneal catheter can be considered in end-of-life care, as they carry a risk of infection making their role limited outside of palliative relief of symptoms in end-of-life care.
3. What is in the pipeline?
- Sodium-glucose co-transporter 2 inhibitors (SGLT2 inhibitors; theoretically these medications can be used to reduce sodium reabsorption and protect the kidneys in patients with metabolic dysfunction-associated steatohepatitis-related cirrhosis and type 2 diabetes). Carefully designed trials are needed.
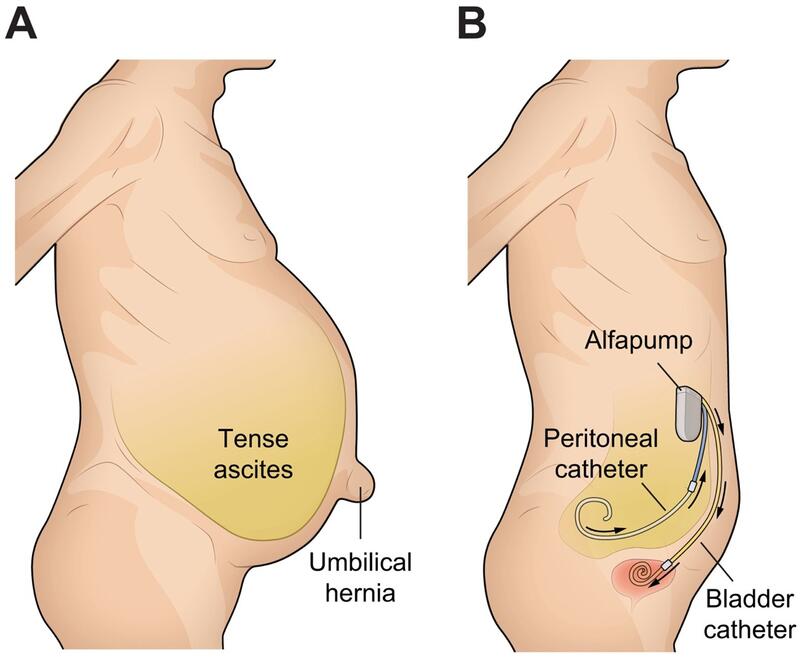
- Low-flow ascites pump (alfapump®) is a subcutaneous device that continuously pumps a small amount of ascites from the peritoneal cavity into the urinary bladder for approximately 16 hr daily during waking hours. Contraindications to the alfapump® are renal dysfunction, loculated ascites, untreatable urinary bladder neck obstruction, recent intra-abdominal surgery, history of urinary bladder cancer, previous solid organ transplantation, hyperbilirubinemia (> 5 mg/dl) and life expectancy less than 3 months. In a recent meta-analysis, survival was the same for patients with alfapump® when compared to patients undergoing LVP. Although, acute kidney injury was frequent in patients with alfapump®. A recent multicenter, single arm study showed controlled ascites and improved quality of life with alfapump® in patients with refractory ascites. Currently, the alfapump® is unavailable in North America.
Fig. 2 Depiction of patient with tense ascites and alfapump® in situ.
Take Home Points:
- Refractory ascites is defined by failure to mobilize ascites despite dietary sodium restriction and maximum tolerated diuretics, or by rapid reaccumulation and/or diuretic-related complications—once present, prognosis is poor.
- Midodrine, an oral alpha-agonist, can be initiated to improve systemic vascular resistance and renal perfusion.
- LVP with albumin infusion remains the cornerstone of symptomatic management, though repeated LVP are associated with worse outcomes compared to TIPS in selected patients.
- TIPS should be considered in appropriate patients as it may reduce ascites burden and improve quality of life.
- Emerging therapies like SGLT2 inhibitors and the alfapump® offer potential future alternatives but are not yet standard care.