Quelling the Swelling
Taken from: Diagnosis, Development, and Treatment of Portal Vein Thrombosis in Patients with and without Cirrhosis. Gastro 2019.
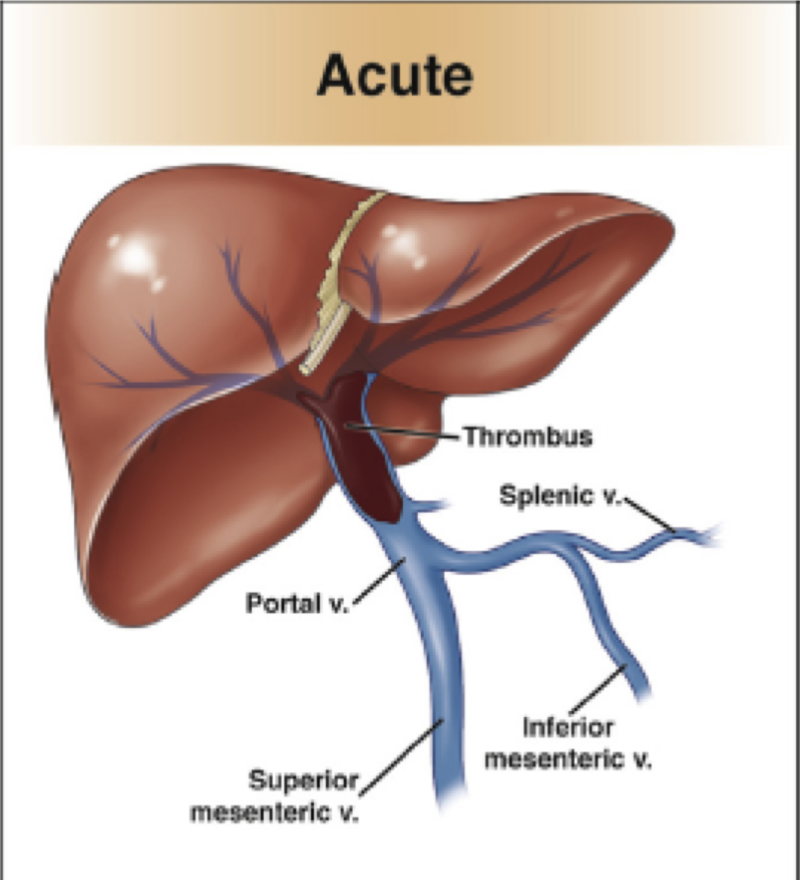
Epidemiology of Acute Portal Vein Thrombosis
The prevalence of acute portal vein thrombosis (PVT) varies in patients with cirrhosis. A wide range exists, with the literature reporting a 2%-23% in this population. The incidence of acute PVT in patients listed for liver transplantation is 7%. Acute PVT is more common in decompensated cirrhosis than well compensated cirrhosis, and the incidence of acute PVT increases over time: in Child-Pugh A and B cirrhosis patients, acute PVT is found in 5%, 8%, and 11% of patients at 1, 3, and 5 years of follow up. Let's return to the case to see how the diagnosis was established.
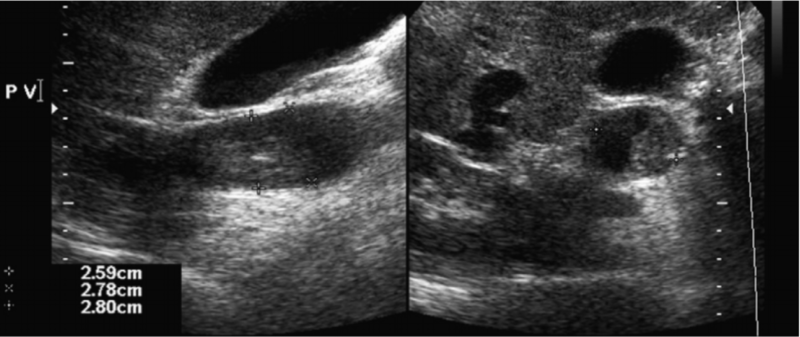
Figure 1 - Acute PVT on ultrasound
Taken from: Thrombosis of the Portal Venous System. Journal of Ultrasound 2007.
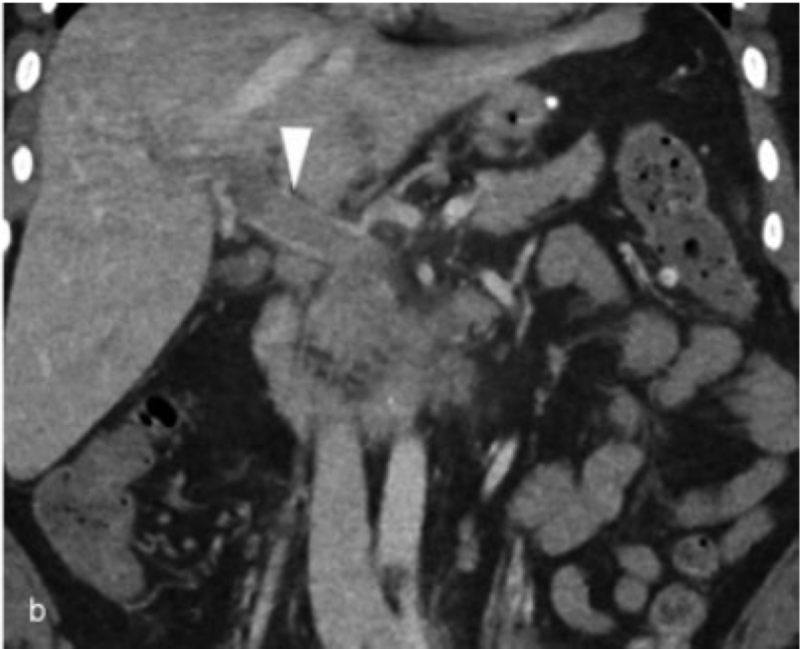
Figure 2a and 2b - Acute PVT on CT
Both images taken from: Acute Portal Vein Thrombosis: Current Trends in Medical and Endovascular Management. Seminars in Interventional Radiology 2018.
Both images taken from: Acute Portal Vein Thrombosis: Current Trends in Medical and Endovascular Management. Seminars in Interventional Radiology 2018.
Risk Factors and Clinical Signs/Symptoms of Acute Portal Vein Thrombosis
Hepatic and extra-hepatic factors can contribute to the development of acute PVT in cirrhosis patients. Hepatic abnormalities linked to cirrhosis, such as portal hypertension, hepatocellular carcinoma (HCC), and portosystemic shunts leading to steal syndrome, are risk factors for PVT. Inherited or acquired thrombophilias, including Factor V Leiden, Protein C and S deficiency, and antithrombin deficiency can also lead to PVT, although these thrombophilias are not routinely checked. The presentation of acute PVT varies. Some patients present asymptomatically, with a diagnosis often made on ultrasound during HCC screening. Extensive clotting in the mesenteric venous system can lead to intestinal infarction and abdominal pain. Ascites secondary to increased portal hypertension can also develop, in addition to variceal bleeding. Of note, contrast is necessary for imaging when assessing for PVT to determine if the PVT is cancer related.
Decision Making in the Management of Acute Portal Vein Thrombosis
Before beginning treatment for acute PVT in patients with cirrhosis, clinicians must first determine if the patient is a candidate for anticoagulation. Important considerations include the following:
- Symptoms
- Liver transplant candidacy
- High risk varices
- Progression of thrombus
If a patient has developed abdominal pain from intestinal ischemia or infarction, initiation of anticoagulation is necessary to prevent further bowel compromise. For patients on the liver transplant waitlist, PVT can lead to a more technically challenging procedure, and although PVT does not worsen pre-transplant mortality, it has been shown to increase post-transplant graft loss and mortality. From a surgical standpoint, the rationale for anticoagulating liver transplant candidates is to improve blood flow to the new graft at the time of transplant, and for these reasons anticoagulation is typically recommended for this subset of patients.
Paradoxically, acute PVT has been associated with higher rates of variceal bleeding, due to elevated levels of portal hypertension. Furthermore, there is not an increased rate of bleeding in cirrhosis patients with acute PVT who are on anticoagulation versus those who are not on anticoagulation. If a decision is made to observe the PVT, repeat imaging is recommended within 1-3 months to assess if spontaneous recanalization has occurred, as up to 40% of acute PVTs are resolved on subsequent imaging. Let's finish the case to see how the patient was managed.
Anticoagulation and Endovascular Therapy
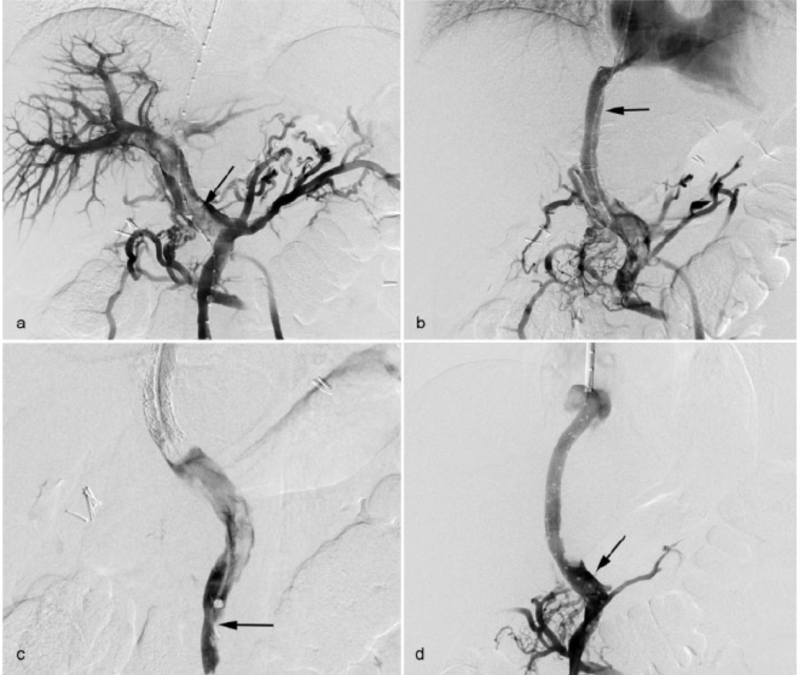
Warfarin, enoxaparin, and direct acting oral anticoagulants such as apixaban have been shown to be successful at recanalizing the portal vein in acute PVT. If the decision is made to anticoagulate, the therapeutic agent should be started within 6 months of diagnosis as initiation of anticoagulation by 6 months improves recanalization rates. According to the latest American Association for the Study of Liver Diseases guidelines, anticoagulation should be started promptly and not held in order for endoscopic variceal ligation to be performed. Treatment duration should be a minimum of six months, with interval imaging every three months, per expert guidance. Consultation with interventional radiology is recommended to determine if endovascular therapy is warranted. Potential therapeutic options include mechanical thrombectomy, directed fibrinolytic therapy, and transjugular intra-hepatic portosystemic shunt (TIPS) placement.
Figure 3 - Interventional radiology venograms of PVT. a: large PVT; b: TIPS implementation; c: mechanical thrombectomy; portal vein with near complete patency, along with TIPS.
Taken from: Acute Portal Vein Thrombosis: Current Trends in Medical and Endovascular Management. Seminars in Interventional Radiology 2018.