Pathology Pearls: Chronic Cellular Rejection
Brief Case Presentation
The patient from the previous Pathology Pearls post (a 50 year old with history of autoimmune hepatitis status-post liver transplant) presents for follow-up two years later. Chart review reveals that three additional hospitalizations for episodes of acute rejection over that time period. Although the patient currently reports no pain or discomfort, there is subtle jaundice on physical exam. Laboratory results are shown in the table below.
| Lab Test | Result |
| AST | 40 U/L (0 – 39 U/L) |
| ALT | 55 U/L (0 – 52 U/L) |
| Alk. Phos | 250 U/L (34 – 104) U/L |
| Total Bilirubin | 4.5 g/dL (0.0 – 1.0 g/dL) |
| Tacrolimus level | 7.1 ng/mL (goal 8 – 10 ng/mL) |
A liver biopsy is performed.
Liver Core Biopsy - Histology Findings
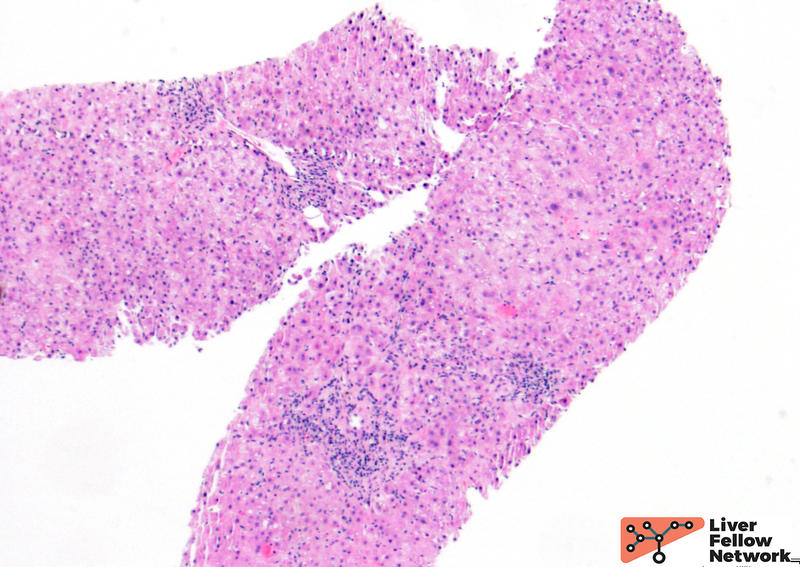
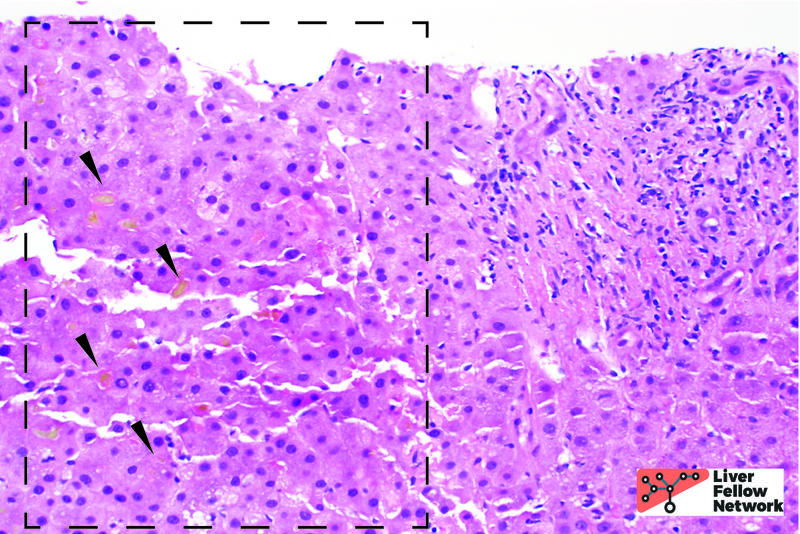
Medium power view of the liver biopsy shows several portal tracts with only mild inflammation (Fig. 1).
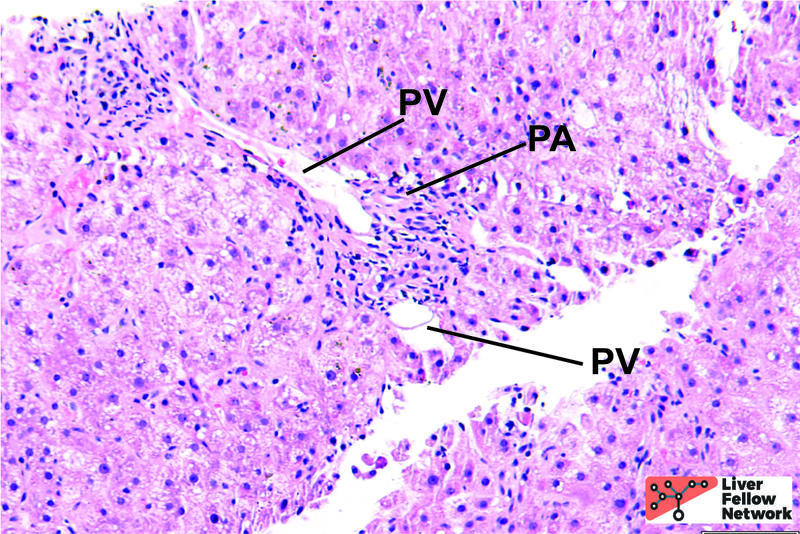
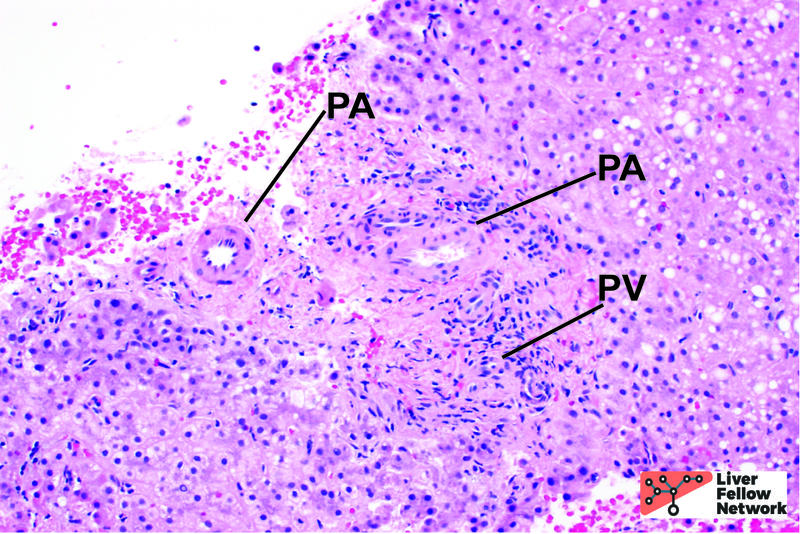
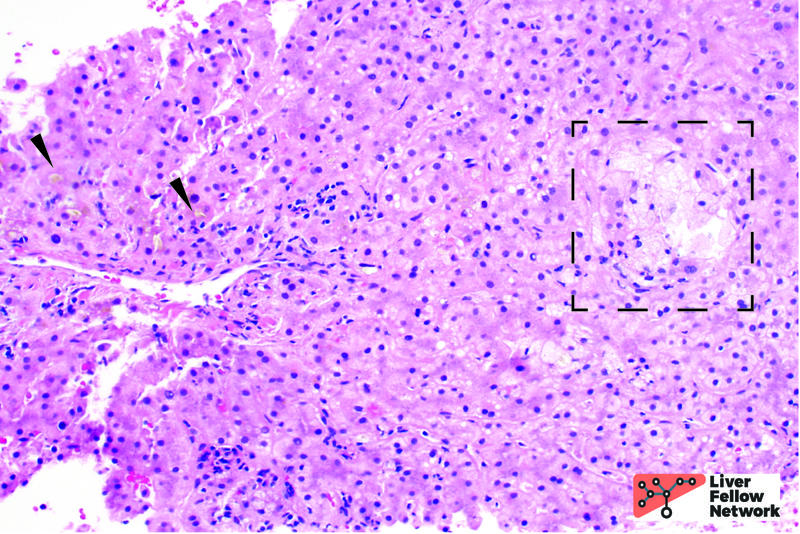
Higher magnification shows portal veins and arterioles, however, there are no visible bile ducts (Fig. 2). Some portal tracts show several unpaired portal arterioles (Fig. 3). For a refresher on the normal histology of the portal tract, see Normal Liver Histology 101.
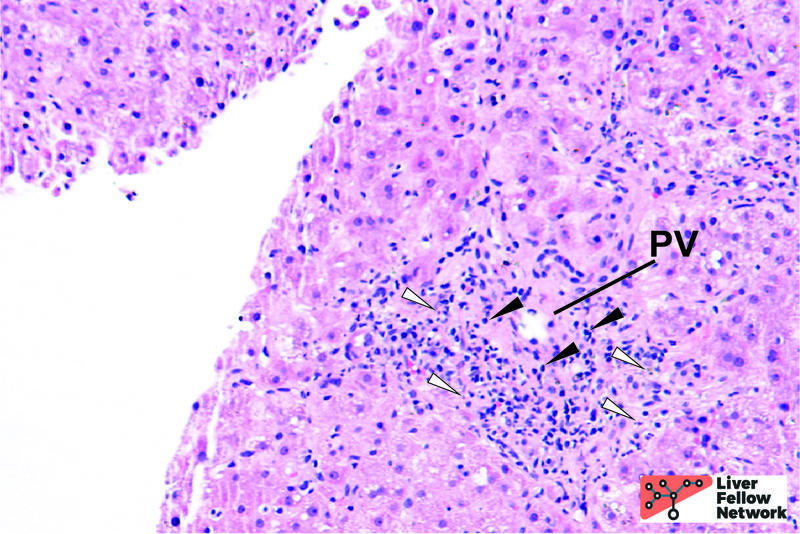
Other portal tracts show mild lymphocytic inflammation, as well as apoptotic debris representing damaged bile ducts (Fig. 4).
The lobules show hepatocellular and canalicular cholestasis (Fig. 5) and there are areas with hepatocytes with cleared out cytoplasm and injury (also known as “cholate stasis”) (Fig. 6).
Taken altogether, the histologic findings in the clinical context are consistent with chronic (ductopenic) cellular rejection.
Chronic cellular rejection (Ductopenic cellular rejection)
Chronic rejection is immune-mediated allograft injury. It is the evolution of multiple, persistent, unresolved episodes of acute T cell rejection. Historically, chronic rejection accounted for 20% or more of liver allograft failures in transplant patients, but that number has decreased dramatically over the past few decades (now ~3%), due to increased recognition and treatment of this type of rejection. Risk factors include donor age above 40 years, recipient age under 30 years, and underlying autoimmune disease necessitating transplant (such as primary biliary cholangitis or autoimmune hepatitis).
The two most specific findings related to chronic rejection are found in the bile ducts or vasculature:
- Biliary: Bile duct loss (ductopenic chronic rejection)
- Vascular: foam cell arteriopathy of medium to large size vessels**
Bile duct loss can be secondary to direct immune-mediated damage, or secondary to ischemic injury due to vascular chronic rejection. Early in the disease process, the histologic picture is similar to that of acute cellular rejection (link to previous post) with lymphocytic ductitis and biliary epithelial damage (loss of polarity, eosinophilic cytoplasm, and epithelial atrophy). The criteria for chronic ductopenic rejection is met when greater than half (>50%) of portal tracts have lost bile ducts. Naturally, loss of bile ducts will lead to hepatocellular and canalicular cholestasis.
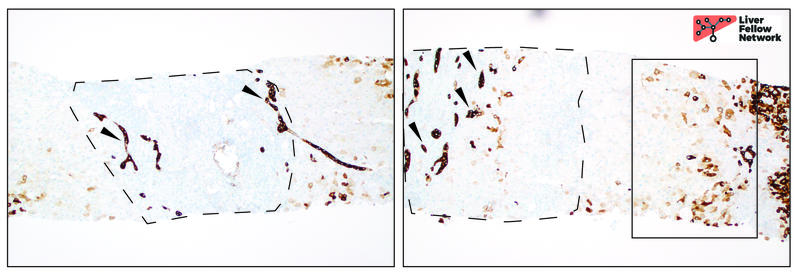
CK7 is a useful immunohistochemical stain to use to evaluate chronic rejection. CK7 will highlight native bile ducts and ductular proliferation. Furthremore, CK7 will reveal hepatocyte that have undergone a process called “cholangiolar metaplasia;” an adaptive response to protect hepatocytes from chronic cholestasis, providing evidence of the chronicity of the disease process. Figure 7 shows an example of CK7 staining in chronic allograft rejection.
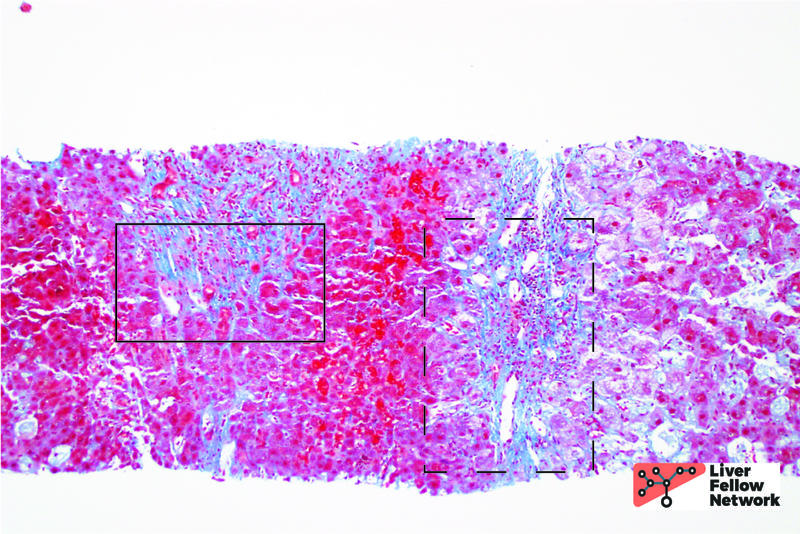
Late stage and severe cases will show centrilobular necrosis (due to chronic ischemia from vascular rejection) and varying fibrosis. Figure 8 shows an example of moderate peri-portal and peri-cellular fibrosis in a case of chronic rejection.
**Of note: this discussion focuses almost entirely on the biliary findings for chronic rejection. The vascular manifestation of chronic rejection (foam cell arteriopathy) is almost never seen on biopsy specimens (you can visit this link from University of Pittsburgh Medical Center to see an example). Foam cell arteriopathy can more often be seen in evaluation of a resected failed allograft or at autopsy.
Differential Diagnosis
The two main findings on liver biopsy for chronic ductopenic rejection are ductopenia and cholestasis. The differential diagnosis, therefore, includes other cholestatic and ductopenic disorders
Chronic biliary obstruction is the most common differential. Obstruction may show portal edema and can often show a more brisk ductular proliferation than chronic rejection (which will show relatively low ductular reaction). However, obstruction, if chronic, can lead to ductopenia, so there can be significant overlap in the histologic picture. Toxic drug induced liver injury (DILI) can often show cholestasis and biliary injury. In most cases, frank ductopenia is not usually seen in DILI, however, certain medications (several antibiotics) have been associated with so-called “Vanishing Duct Syndrome.” Recurrence of autoimmune biliary disease, such as primary biliary cholangitis (PBC) or primary sclerosing cholangitis (PSC) should also be considered.
References
- Torbenson, Surgical Pathology of the Liver. 2018.
- Burt, MacSween’s Pathology of the Liver: Seventh Edition. 2017.
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Vanishing Bile Duct Syndrome. Updated December 11, 2019.
Acknowledgements
Special thanks to Dr. Nigar Khurram for providing images for Figures 1, 2 and 4.