Pathology Pearls: Evaluation of Donor Liver Biopsies
Brief Case Presentation
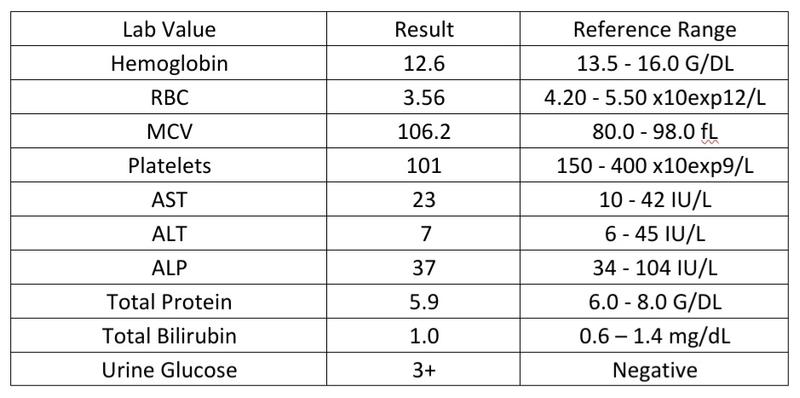
A 57 year old male with past medical history of alcohol use presented to the emergency department with altered mental status. The patient was in his usual state of health the morning before and called EMS with severe headache. He lost consciousness on the way to the hospital and airway protection was provided en route. A CT scan of the head showed a pontine hemorrhage. The poor prognosis for his hemorrhage given it's location was discussed with the family who agreed he would not want to live in a nursing facility dependent on care and was found to be an organ donor. The pertinent lab values were as follows:
A liver wedge biopsy was sent to pathology for frozen section to evaluate for potential liver donation.
Liver biopsy findings
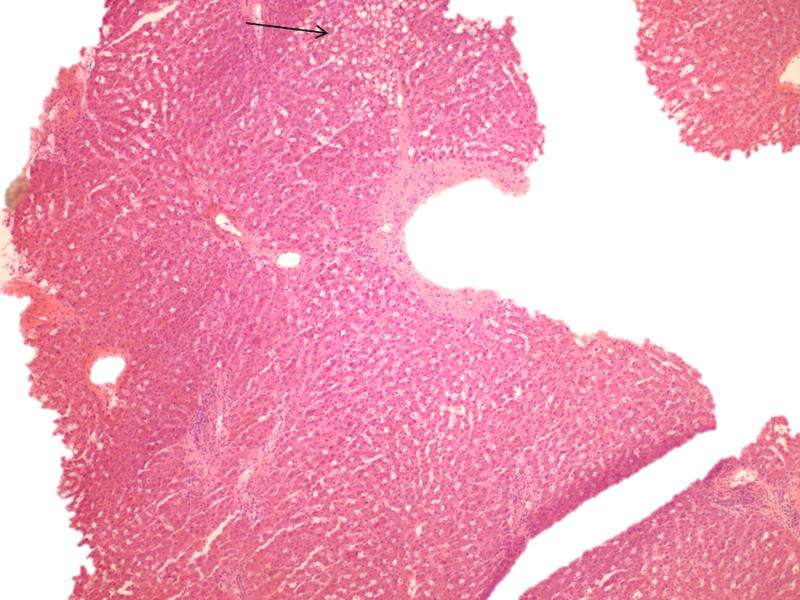
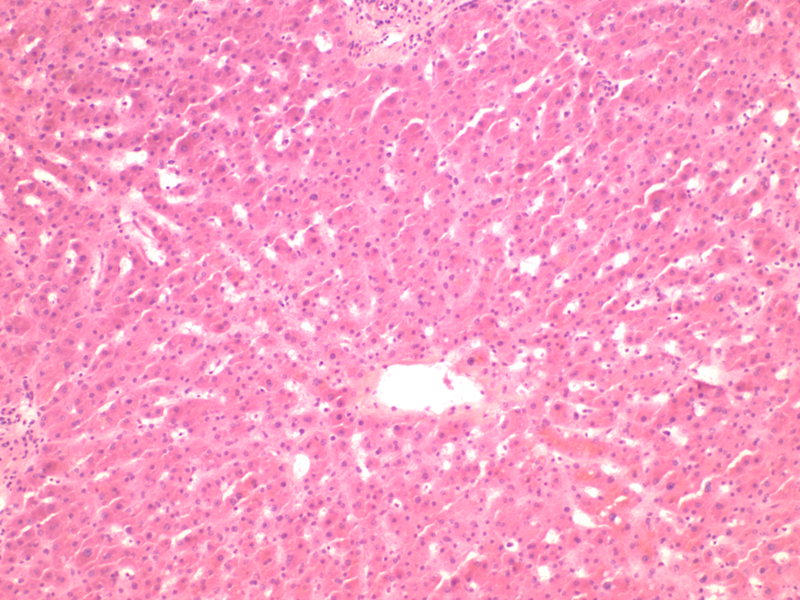
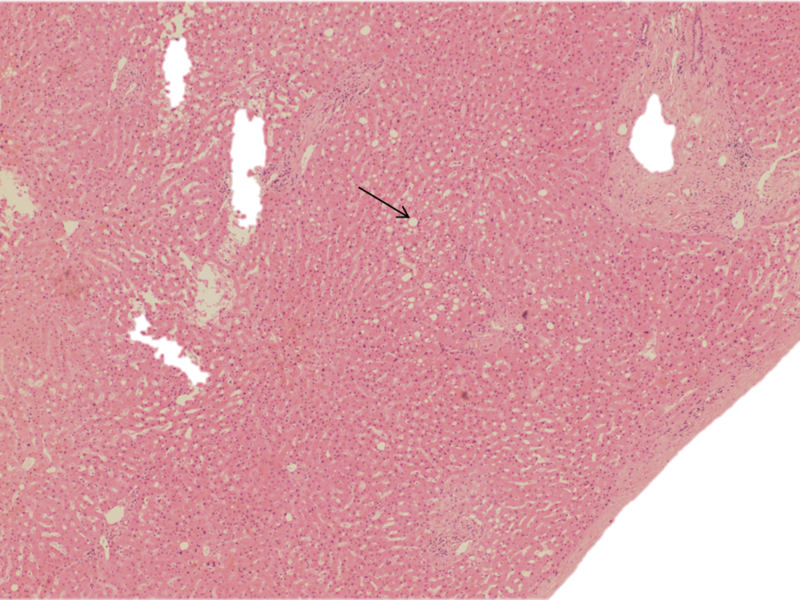
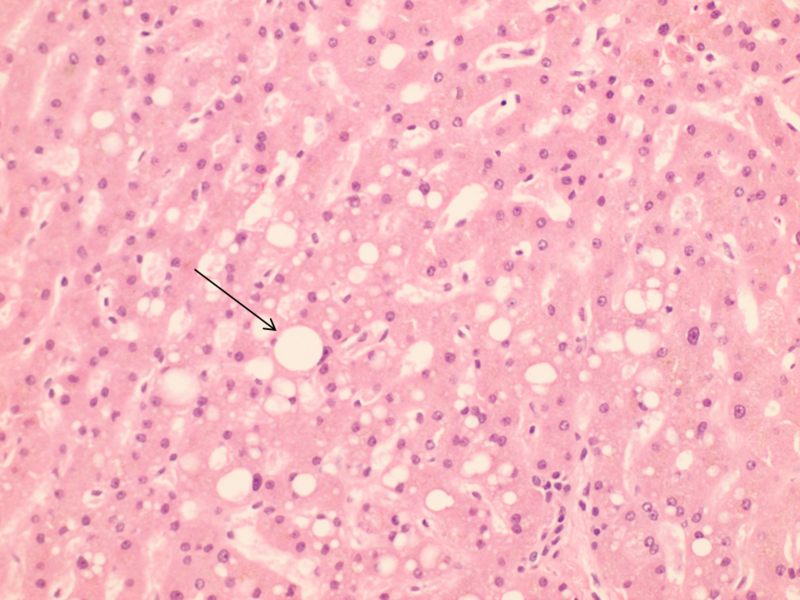
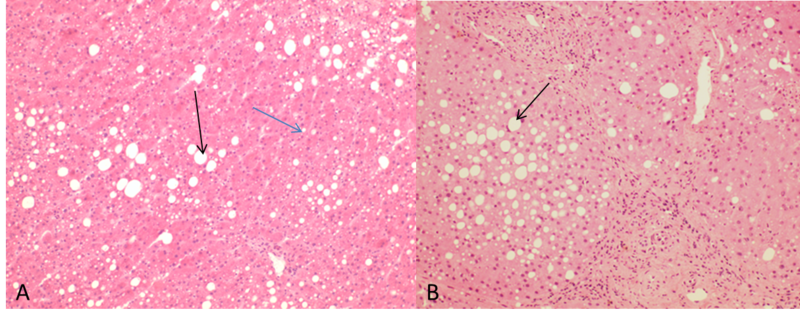
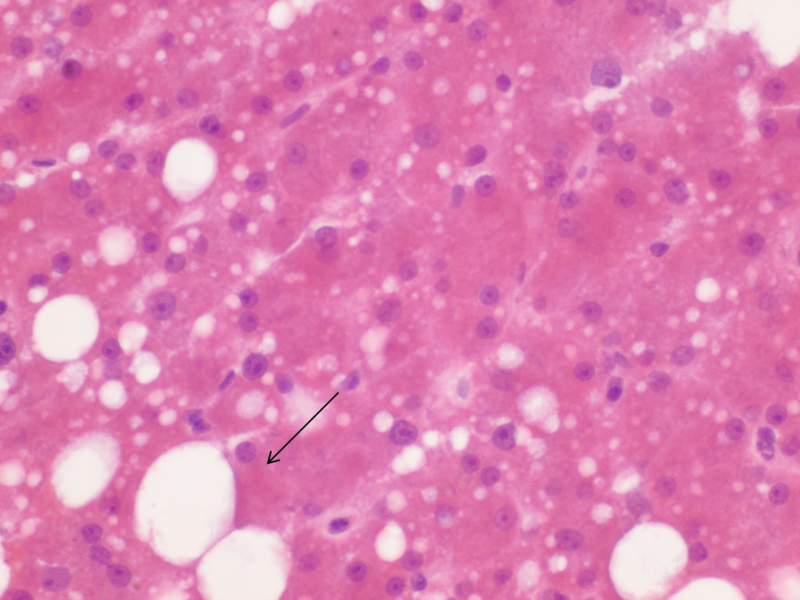
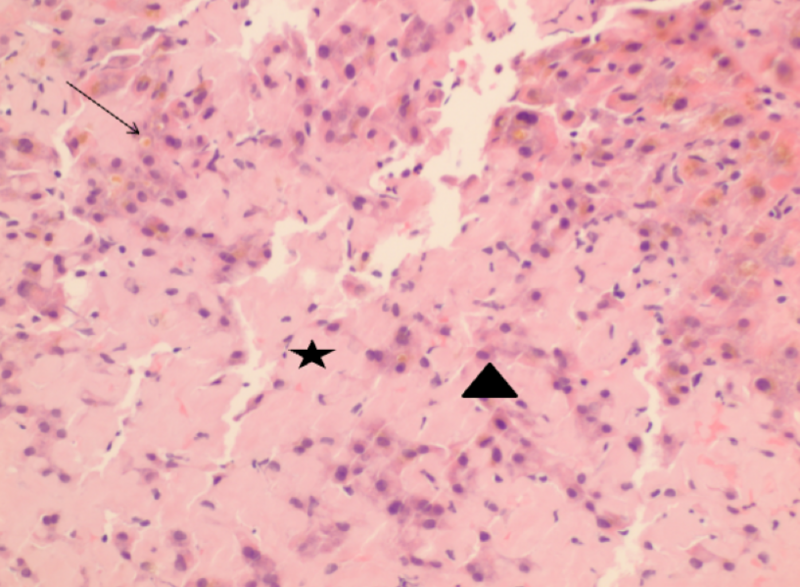
At low power, the hepatic parenchyma displayed benign polygonal, eosinophilic hepatocytes with <5% macrovesicular steatosis and 15% microvesicular steatosis (Figure 1). There was no congestion or hemorrhage. No single cell or confluent necrosis was seen. Cholestasis was absent. No inflammation was found within the lobules (Figure 2). Zone 3 (Centrilobular) lipofuscin depositions was seen.
The portal tracts displayed mild lymphocytic inflammation. No vascular thrombi were identified and there was no Bile duct damage or proliferation.
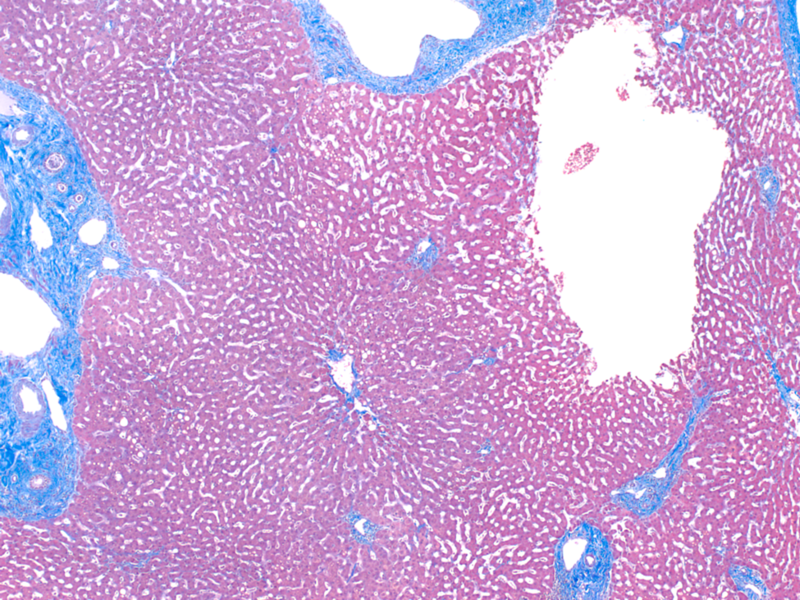
Additionally, no fibrosis was identified.
The tissue was subsequently sent for permanent sections for evaluation of H&E stained sections.
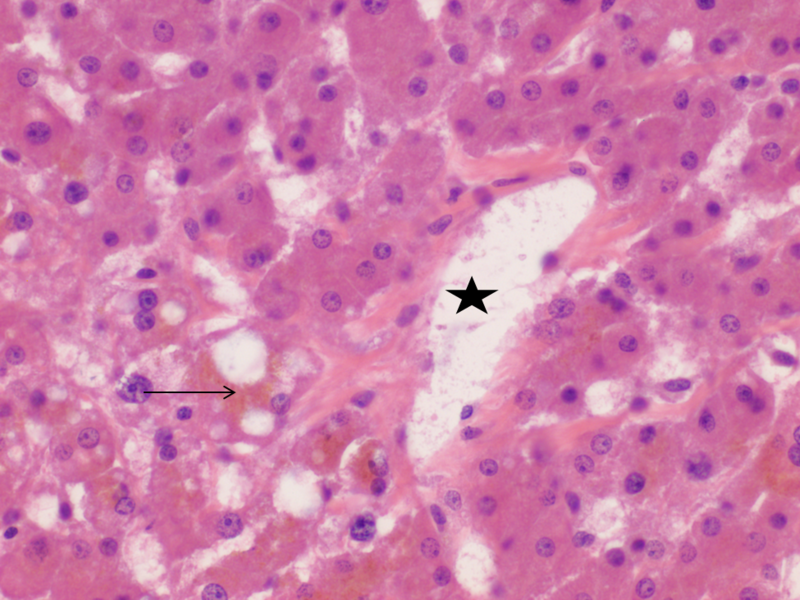
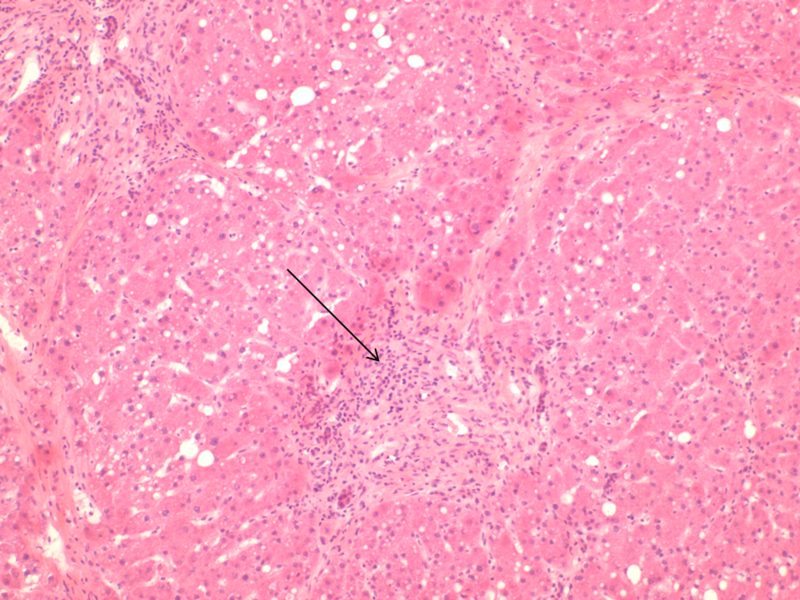
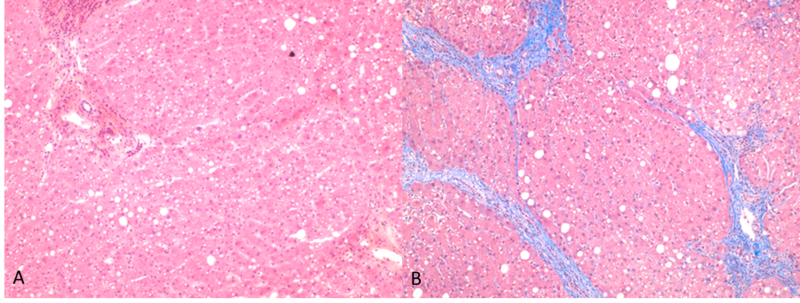
On H&E stained sections (Figure 4) the subcapsular liver parenchyma displayed 1-2% large droplet macrovesicular steatosis (Figure 5). No chronic inflammation was seen in portal, periportal or lobular areas. No fibrosis was seen in portal, periportal and lobular areas (Figure 6). There was no evidence of bile duct injury.
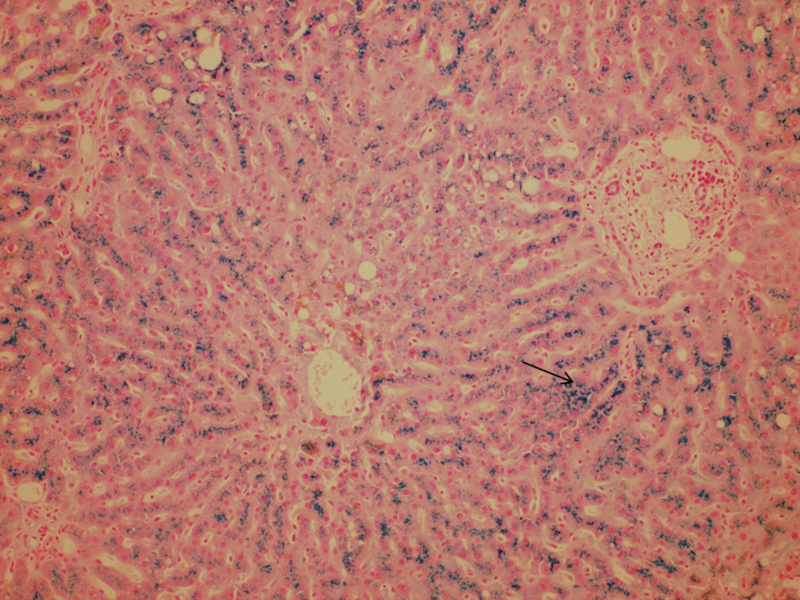
An iron stain displayed marked hepatocellular iron deposit, 4/4 (Figure 7). This was reported to the clinical team as suspicious of genetic iron deposit disease, such as hemochromatosis. Genetic correlation was advised.
Donor Liver Evaluation
The evaluation of donor liver biopsies and the use of marginally acceptable livers varies between liver centers around the world. The liver biopsy can provide useful information regarding the health of the liver prior to the transplant. Several factors come into consideration prior to acceptance of a donor liver such as age of the deceased donor, cause of death, amount of warm ischemia time, cold ischemia time, gross appearance of the liver, status of the recipient and the histological findings at donor evaluation through frozen sections.
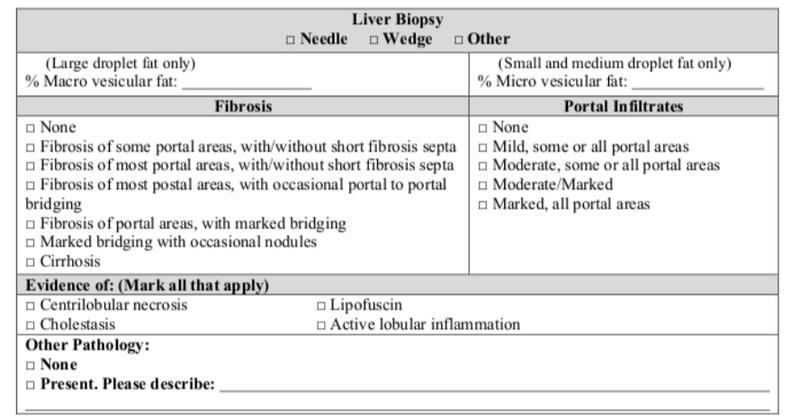
The pathologists’ job is to identify and report steatosis, inflammation, necrosis, and fibrosis. Other significant findings should also be reported.
Steatosis
Only macrovesicular steatosis is scored as smaller droplet fat has minimal or no effect on outcomes. Marked or severe macrovesicular steatosis of the donor liver is associated with early allograft dysfunction, primary non-function, and postreperfusion syndrome. Over the years various ways of reporting this large droplet fat have been used such as mild/moderate/severe or percentage of hepatocytes involved. The biennial Banff Conferences on Allograft Pathology convene pathologists, physicians, surgeons, and immunologists with the goal of producing consensus guidelines for standardizing the assessment of allograft biopsies. The most recent Banff guidelines for steatosis agreed on the reporting of large droplet subset of macrovesicular steatosis. The percentage of steatosis to be reported should be assessed on low power magnification. This should be followed by a high power assessment of the fat rich areas to ensure that only large droplet fat percentage is reported. Large droplet fat was described by most as a single droplet of fat expanding the hepatocyte and displacing the nucleus and therefore, the fat droplet should be at least slightly larger than adjacent hepatocytes, which contained no fat or small fat droplets. Smaller droplets than this were considered small droplet macrovesicular fat. On the other hand microvesicular fat is described as distended hepatocytes with foamy appearing cytoplasm; small lipid vesicles (less than 1µm in diameter) that may or may not be discernible along with a centrally located nucleus.
Other factors that may explain variation in the scoring of the steatosis are :
1) Gradual variation in the size of fat globules making it difficult to score (Figure 8);
2) Inherent difficulties in assessing steatosis on frozen sections and recognizing the cell membrane of non-steatotic hepatocytes to compare fat droplet size (this is particularly difficult when there are mixed medium and large droplets present)( Figure 9);
3) The fact that the assessment of a percent of a subset of fat droplets within irregularly shaped areas in an irregularly shaped biopsy is not easy for the human brain to compute;
4) Variation in frozen section tissue thickness (5-6-μm-thick sections are recommended because thinner sections tend to overestimate whereas thicker (>8-10 μm) tend to underestimate the severity of Large droplet fat).
Inflammation
The inflammation can be scored as minimal to marked, with the portal and lobular inflammation evaluated separately. A formal grading system for inflammation (e.g., Ishak score) is also acceptable but not necessary. Donor livers commonly show minimal to mild nonspecific inflammation, but moderate (Figure 10) or greater inflammation suggests an underlying liver disease.
Necrosis
When present, necrosis is usually focal and mild and located in zone 3 or is immediately beneath the liver capsule. Necrosis should be estimated to the nearest 10% and the location provided.
Fibrosis
Fibrosis is staged in the usual fashion (pericellular, portal, bridging, cirrhosis).
Other Findings
Examples include granulomas, excess pigment that suggests iron, cholestasis, amyloidosis etc
References
- Torbenson, Atlas of Liver Pathology: A Pattern-Based Approach. 2019
- Burt, MacSween’s Pathology of the Liver: Seventh Edition. 2017.
- Neil, DAH, Minervini, M, Smith, ML, Hubscher, SG, Brunt, EM, Demetris, AJ. Banff consensus recommendations for steatosis assessment in donor livers. Hepatology. 2022; 75: 1014– 1025
- Markin RS, Wisecarver JL, Radio SJ, Stratta RJ, Langnas AN, Hirst K, et al. Frozen section evaluation of donor livers before transplantation. Transplantation. 1993;56(6):1403–9