The Coagulopathy of Liver Disease -- Part 2
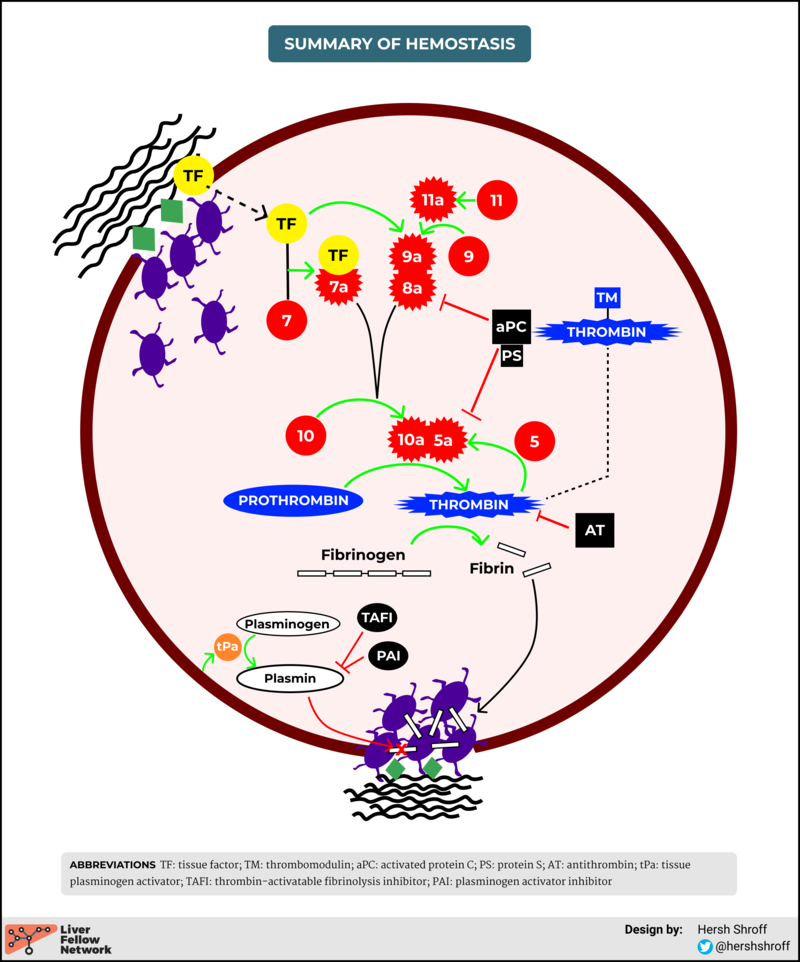
In my last post, we discussed normal hemostasis. Figure 1 shows a visual summary of all of the steps in the hemostatic process that we discussed in that post.
Figure 1: Summary of Hemostasis
In today's post, we’ll go back through the various stages above and discuss the important physiological changes that happen in cirrhosis.
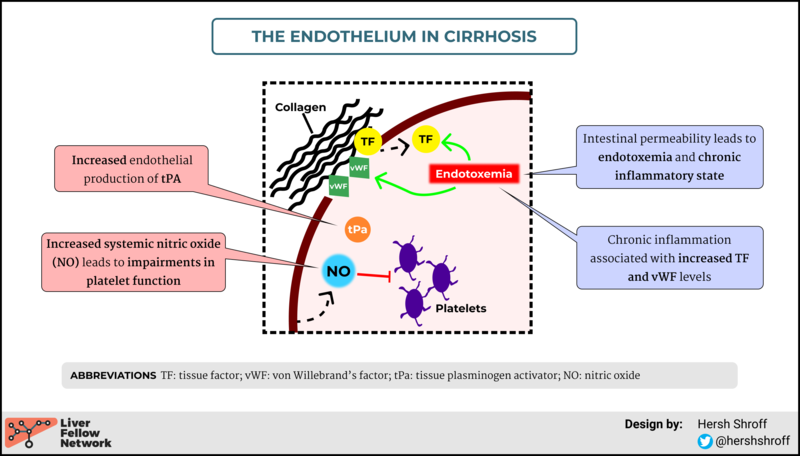
Endothelial abnormalities in cirrhosis
Read more:
- Vascular endothelial dysfunction in cirrhosis leads to increased systemic and splanchnic nitric oxide, which affects platelet function
- Cirrhosis = increased intestinal permeability = endotoxemia and chronic inflammation = increased TF and vWF
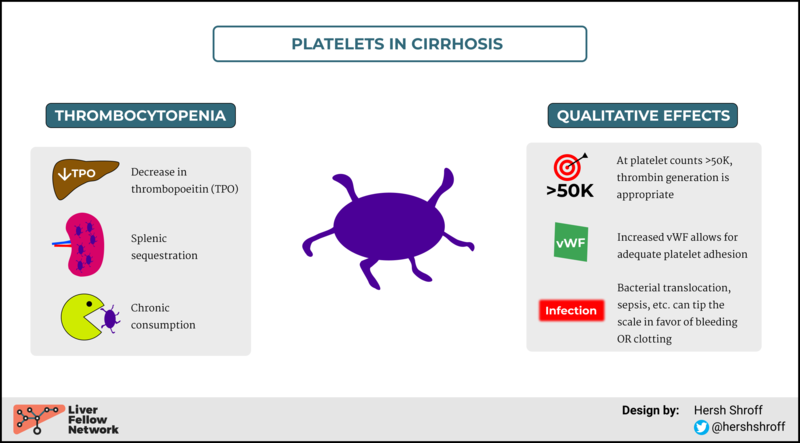
Platelet changes
Read more:
Violi et al. provide a terrific review of platelets in liver disease, reviewing many of the concepts illustrated above.
One important takeaway here is that while we all know that platelet numbers are clearly reduced in cirrhosis, the qualitative changes are much harder to pinpoint. In a very clever study by Tripodi and colleagues, they were able to show that in patients with cirrhosis thrombin generation (which is the ultimate goal of the hemostatic process) remained adequate above platelet counts of 50,000. At the same time, the overall state of the patient’s liver disease and the presence of clinical events -- namely overt infection, but also endotoxemia, bacterial translocation, variceal bleeding, malignancy -- can take a seemingly well-functioning platelet and throw it into disarray. There can be wild, unpredictable disruptions to the tenuous balance, shifting the scale towards bleeding and/or clotting. Dr. Tapper illustrates this nicely, and teaches us about the exhausted platelet, here.
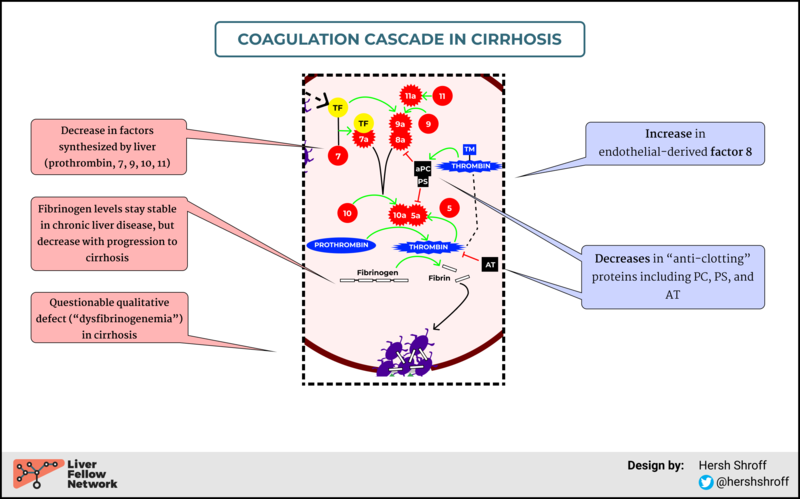
Coagulation cascade abnormalities
Read more:
- Despite a loss of many coagulation factors, the acquired protein C deficiency in cirrhosis appears to play an important role in the observed hypercoagulability of these patients
- An increase in endothelial-derived factor VIII may also contribute
- As liver disease progresses, changes in fibrinogen levels can be seen
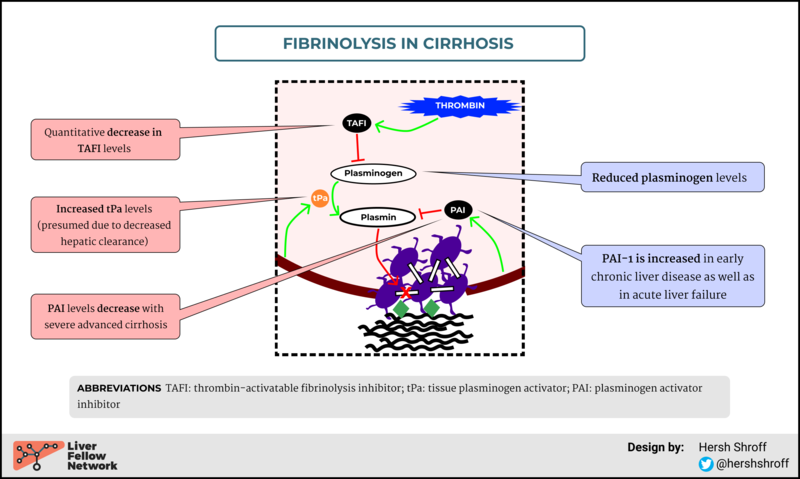
Alterations in fibrinolysis
Read more:
- Remember what we talked about in Post 1 about fibrinolysis: TAFI and PAI-1 inhibit plasmin, thereby reducing fibrinolysis
- On the left in the above figure, the decrease in TAFI and PAI-1 (in advanced liver disease), removes the inhibition of plasmin, creating a hyperfibrinolytic state.
- In cirrhosis, we also see increased tPA levels
- PAI-1 is interesting as it can increase and decrease in various stages (higher in early chronic liver disease and acute liver failure, but lower with advanced chronic liver disease)
Summary
The really high level summary here is this -- lots of changes occur on a physiologic level. Some favor bleeding. Others favor clotting. What results is a rebalanced, yet very tenuous, state of hemostasis that is dramatically affected by the overall health state of your patient. A clinical event (usually infection) can dramatically alter this balance.
In upcoming posts, we’ll hopefully get out of the weeds and start answering some clinically relevant questions. How are tests of bleeding/clotting affected by cirrhosis? When do we need to give transfusions?
Stay tuned!