Why are non-invasive risk scores such as FIB-4 used in clinical practice?
One of the most important predictors of liver related morbidity and mortality is stage of liver fibrosis. This makes identifying and quantifying the degree of fibrosis extremely important to risk-stratify patients and determine who needs further evaluation and treatment of liver disease.
The current gold standard for determining hepatic histology is a liver biopsy, but biopsies are invasive, uncomfortable, and time consuming for patients. There are several other cons to liver biopsies including risk of complications ranging from pain at the biopsy site to more life-threatening complications such as biliary leak, bleeding, and pneumothorax. Biopsy results depend on pathologist interpretation and are subject to variations in interpretation of biopsy results and results may take several days to come back, so do not provide information at the point of care. Additionally, there may be sampling error—a biopsy taken in one location of the liver may not be representative of pathology in the whole liver.
Because of the limitations of liver biopsies there is a lot of interest in non-invasive tools to detect and monitor for liver fibrosis. These non-invasive tests boil down into two main categories: imaging and risk scores.
There are several imaging modalities including MRE, vibration controlled transient elastography (VCTE) that are used for assessment of fibrosis. VCTE uses wave velocity to indicate liver stiffness measurement, but sensitivity is decreased in obesity, non-fasting states, and cardiac congestion. MRE uses acoustic shear waves and cross-sectional images to detect fibrosis but can be expensive and is contraindicated in some patients with pacemakers. In general, both are great noninvasive tools but can be expensive and may not be readily accessible to all patients.
Enter: Non-invasive risk scores!
Who is using non-invasive risk scores?
Ideally these risk scores will be used by primary care providers to help determine who needs referral to a hepatologist for further management. This is an important way to identify patients that may have more advanced liver disease and get them the specialty attention they need. Therefore, a good non-invasive screening test will be affordable and will use readily available patient information, such as demographic characteristics and lab parameters. Many hepatologists may also use these risk scores as an initial assessment. If patients’ scores suggest no or minimal fibrosis, they can potentially be managed conservatively, but if their scores suggest fibrosis, they may need additional testing and treatment.
The main advantage of risk scores is that they typically only require the age of the patient and basic labs to calculate. It’s a win-win for clinicians and patients to avoid liver biopsies if they can get similar information from risk scores. An ideal risk score will be easy to use, cheap, and accurate.
There are several risk scores out you may have heard about such as FIB-4 (Fibrosis-4), APRI (AST to platelet ratio index), and NFS (NAFLD fibrosis score). FIB-4 is the most used, so let’s do a deep dive into its origins…
Where did FIB-4 come from?
The creators of the FIB-4 score originally found that the score helped predict significant fibrosis in patients with HIV and Hepatitis C co-infection. The authors performed a retrospective analysis of liver histology and baseline clinical parameters in 832 patients with HIV/HCV co-infection. Patients were categorized into 3 fibrosis strata (mild, moderate, and advanced) based on liver biopsy pathology and subjects were divided into training and validation sets.
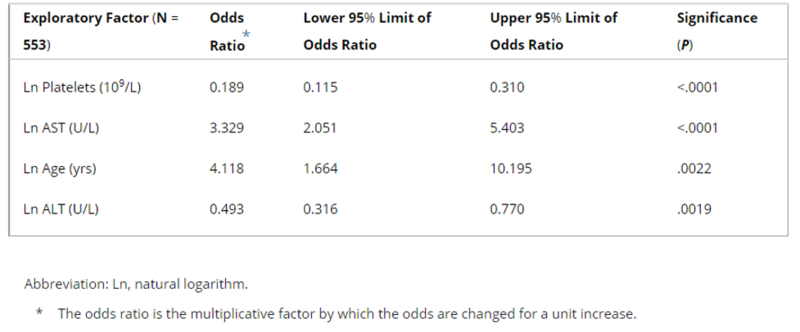
Multivariate logistic regression analysis demonstrated a significant association between platelet count, age, AST, and ALT with fibrosis in the study population as seen in the table below.
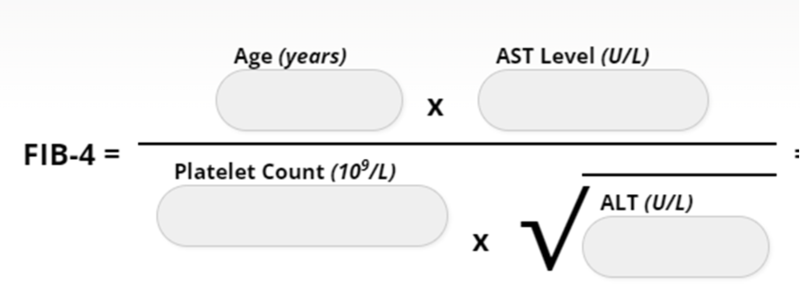
Using these variables, the FIB-4 index was derived:
The area under the receiver operating characteristics (AUROC) using FIB-4 was 0.765 for differentiation between fibrosis score (Ishak stage) 0–3 and 4–6. Using a cutoff of < 1.45 the FIB-4 score had a negative predictive value of 90% for advanced fibrosis with a sensitivity of 70%. FIB-4 scores greater than 3.25 had a positive predictive value of 65% for advanced fibrosis in the validation group. The authors argued that liver biopsy could be avoided in the patients with FIB-4 scores <1.45 or >3.25 with correct fibrosis classification in 87% of these subjects.
One of the great things about FIB-4 is that it is simple and the labs that are needed are readily available in most patients. The score calculator seen above can easily be pulled up on a computer or phone when in clinic.
But what are the pitfalls of FIB-4?
There are a few pitfalls of the FIB-4 score. First, it was developed in a cohort of patients with an average age around 40 years old and there is evidence that it does not perform as well at young or old age extremes. One study found that the specificity of FIB-4 for advanced fibrosis decreases with increasing age with a specificity of less than 30% with age greater than 65, leading to false positives in older patients.
The score is reliant on lab values so other conditions that raise or lower AST, ALT, and platelet count can make FIB-4 inaccurate. For example, exposures that raise AST such as alcohol can also increase the FIB-4 score, potentially resulting in false positives. Patients with low platelets from etiologies other than portal hypertension such as medications, immune thrombocytopenia, and viruses may also overestimate FIB-4 and lead to false positives. It is important to keep these things in mind when interpreting your patients FIB-4 score.
The score was also initially developed in patients with HIV/HCV infection so the cutoffs of 1.45 and 3.25 are specific to this population and may not be generalizable to patients with different etiologies of liver disease.
Why is FIB-4 used in NAFLD?
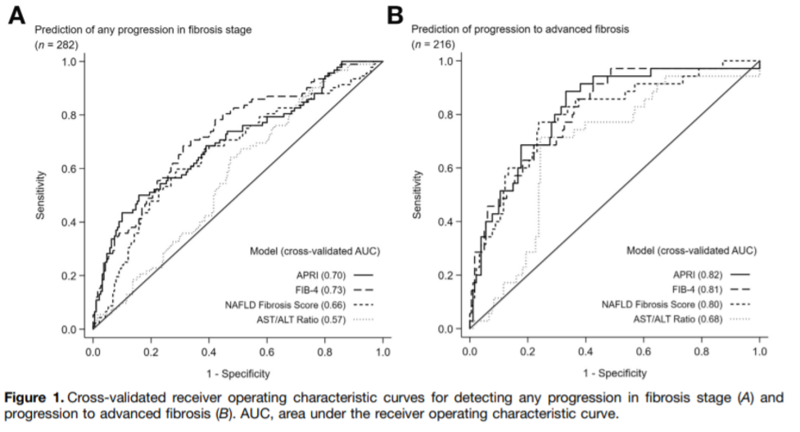
You may have heard that FIB-4 scores are most often used in the clinical setting of non-alcoholic steatohepatitis. Siddiqui et al. performed a cross-sectional study to determine the diagnostic utility of FIB-4 scores in a large, diverse population with NAFLD over time. The study found that the FIB-4 score was able to predict advanced fibrosis in patients with NAFLD with a c-statistic of 0.80 and to predict progression to advanced fibrosis over time with a c-statistic of 0.81. For advanced fibrosis, the cutoffs for 90% sensitivity is 1.02 was and 90% specificity is 1.95 with a prevalence of advanced fibrosis of 28% of the 1904 individuals in the cohort.
The authors also evaluated the diagnostic ability of other risk scores including APRI, NFS, and AST/ALT Ratio and found that NFS and APRI were also able to detect fibrosis and predict progression to fibrosis in NAFLD.
So what cutoffs are used in NAFLD?
In another study using a database with 541 people with NAFLD, a FIB-4 score greater than or equal to 2.67 had an 80% positive predictive value and a FIB-4 score less than or equal to 1.30 had a 90% negative predictive value. These are the scores that are generally used in clinical practice to rule someone in or out for advanced fibrosis.
How does FIB-4 perform?
Researchers have proposed the FIB-4 score be used by primary care physicians with NAFLD to determine who might need further referral to a specialist. In a study by Davyduke, adult patients with elevated ALT and/or steatosis on imaging without a previous liver diagnosis underwent vibration-controlled transient elastography (VCTE) and had FIB-4 scores calculated. Decision modeling identified a FIB-4 score of 1.3 was an inflection point where probability of high liver stiffness measurement was over 12.5%. FIB-4 scores of less than 1.3 excluded the presence of advanced fibrosis in 89% of patients. The authors argue using a two-step approach of FIB-4 score first could eliminate the need for 87% VCTE examinations and prevent hepatology referrals in 69% of cases. However, FIB-4 alone with scores of less than 1.3 would miss over 8% of at-risk patients with high liver stiffness measurement. The study found that FIB-4 can help identify patients with NAFLD that may be at higher risk of advanced fibrosis that may benefit from further hepatology evaluation as well as “rule out” patients at low risk. However, this study showed that FIB-4 isn’t perfect and may miss a number of patients that truly have advanced fibrosis and is better when combined with VCTE. Other studies have similarly found that FIB-4 plus VCTE improves the specificity in detecting advanced fibrosis. The study authors recommended using a staged approach with FIB-4 score and VCTE to risk-stratify patients with NAFLD, although notably VCTE is expensive and may not be readily available to most primary care providers.
In another study by Graupera et al., a FIB-4 score of greater than 2.7 correlated with a liver stiffness measurement greater than or equal to 8 kPa in 83% of the at-risk patients in the study and 67% with a liver stiffness measurement above 12 kPa. However, the study also highlighted that several subjects with high-risk clinical conditions such as diabetes and obesity had a large number of false negative results (11% of diabetic patients) with FIB-4 score alone.
Researchers have also looked at repeat FIB-4 measurements to identify individuals at risk of cirrhosis over time. In a Swedish cohort, FIB-4 score was calculated twice over a 5-year period and found that individuals with a 1 unit increase in FIB-4 score between the measurements was associated with an increased risk of advanced fibrosis, thereby helping to increase the sensitivity of the FIB-4 score overall. A subsequent study found that increase in FIB-4 scores over time is associated with increased risk of disease progression and higher baseline scores experienced higher rates of disease progression to cirrhosis. Despite improved detection of advanced fibrosis with repeat scores, the sensitivity of FIB-4 score remains too low to recommend as a screening test.
Take away: FIB-4 can be useful in guiding primary care physicians and hepatologists to determine if further diagnostics are needed in individuals found to have NAFLD with the caveat that FIB-4 may miss some patients with high liver stiffness measurements and extra caution should be used in interpreting these scores in patients with diabetes or obesity, or in the very young or old.
How do I use FIB-4 in practice?
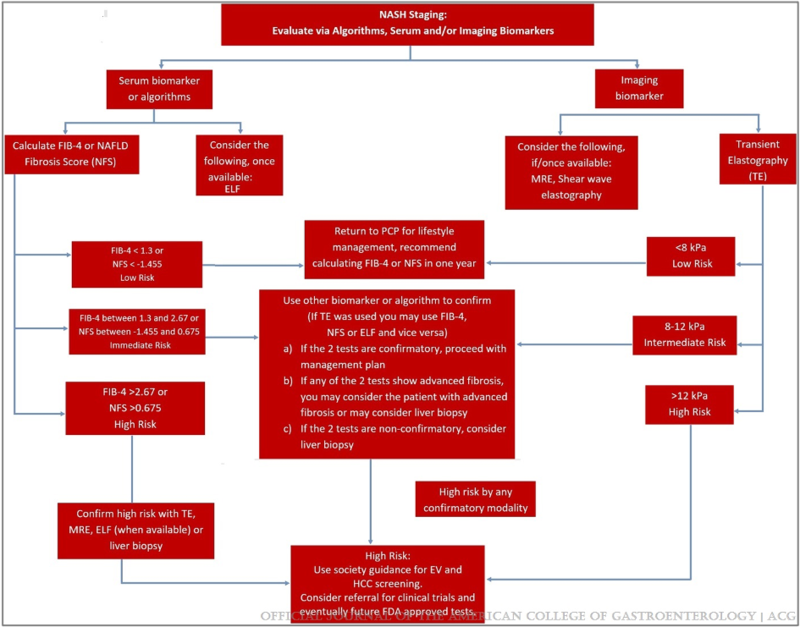
The American College of Gastroenterology and the Chronic Liver Disease Foundation put together an expert panel to create a practical algorithm to identify patients at high risk of NASH to help the practicing gastroenterologist that sheds some light on how some of the experts use FIB-4 in practice:
What other non-invasive risk scores are out there?
There are other non-invasive risk scores that are used in clinical practice that can also provide useful information about fibrosis risk. These include APRI, NFS, AST/ALT ratio. We will save the discussion of the pros and cons of these other noninvasive tests for a future post.
Although FIB-4 scores are clinically useful and obviate the need for liver biopsies in many patients with NAFLD, there is still room for improvement in this risk score so that it has more accurate positive and negative predictive values for determining advanced fibrosis for people of all ages. Here’s to hoping that researchers continue to improve upon noninvasive risk scores in the future to make for even better tools to diagnose and manage advanced fibrosis!