Why does hepatic encephalopathy develop after transjugular intrahepatic portosystemic (TIPS) shunt?
Transjugular intrahepatic portosystemic shunt (TIPS) has become a standard procedure for the treatment of portal hypertension complications. The most common indications include refractory ascites and secondary prevention of variceal bleeding. Refractory ascites has a response rate of up to 85%. In patients with recurrent variceal bleeds and high risk of treatment failure or increased mortality risk, TIPS is a highly effective intervention.
TIPS has improved transplant-free survival and TIPS-associated complications like shunt dysfunction have been markedly reduced. However, incidence of HE after TIPS remains around 30-50%. This is associated with frequent readmissions and increased healthcare costs. In addition, a small number of patients develop refractory HE that requires endovascular interventions and/or liver transplantation.
How does TIPS work? What are the complications?
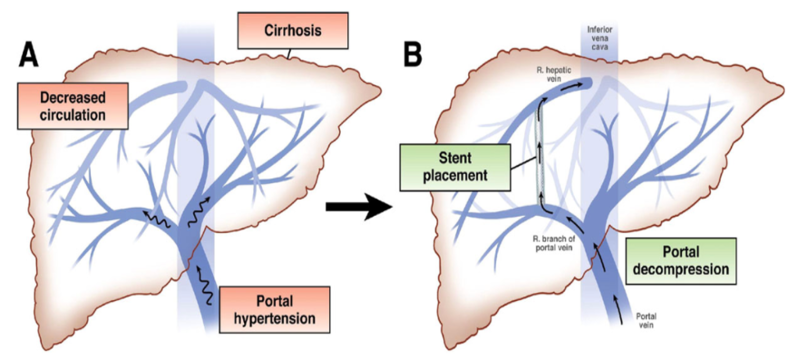
TIPS is a minimally invasive procedure placed via interventional radiology with the purpose to reduce portal hypertension. A needle catheter is passed via the right internal jugular vein to the hepatic vein, and then a tract is made to the intrahepatic portion of the portal vein. The hepatic tract is then dilated and kept patent through deployment of a metal stent.
The main complications of TIPS are hepatic encephalopathy, shunt dysfunction and liver failure. After the discovery of self-expandable metal stents, TIPS rapidly gained acceptance for the treatment of portal hypertension-related complications like variceal bleed, refractory ascites and hepatic hydrothorax. Unfortunately, the uncovered self-expandable metal stents had high rates of shunt dysfunction requiring multiple reinterventions. With the development of expanded-polytetrafluoroethylene covered (e-PTFE) covered stents, the incidence of shunt dysfunction markedly decreased.
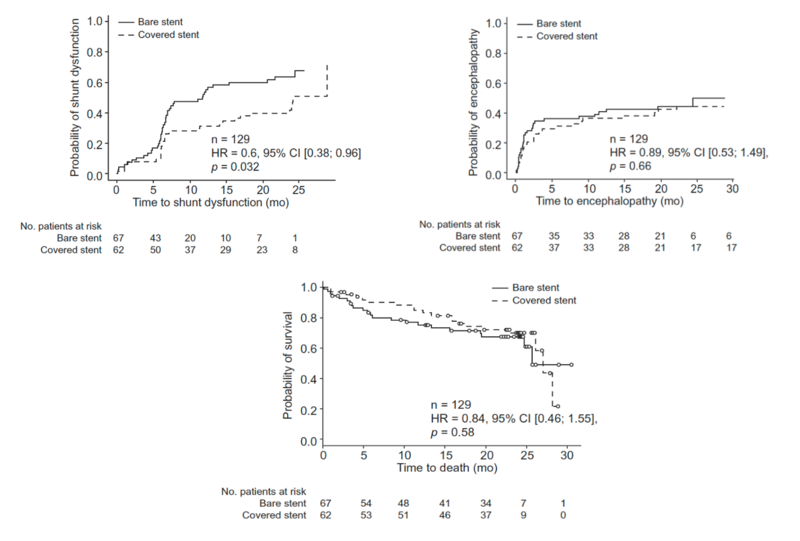
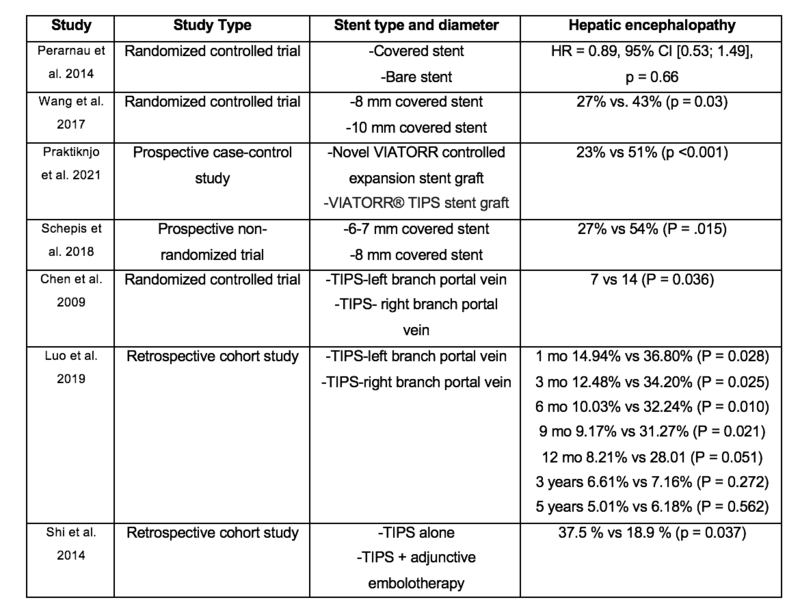
Initial studies suggested an increased risk of HE with the placement of e-PTFE covered stents. However, a study from Perarnau et al from 2014 showed that long-term patency was better for covered stents than bare metal stents, and there was no difference on survival or the incidence of HE.
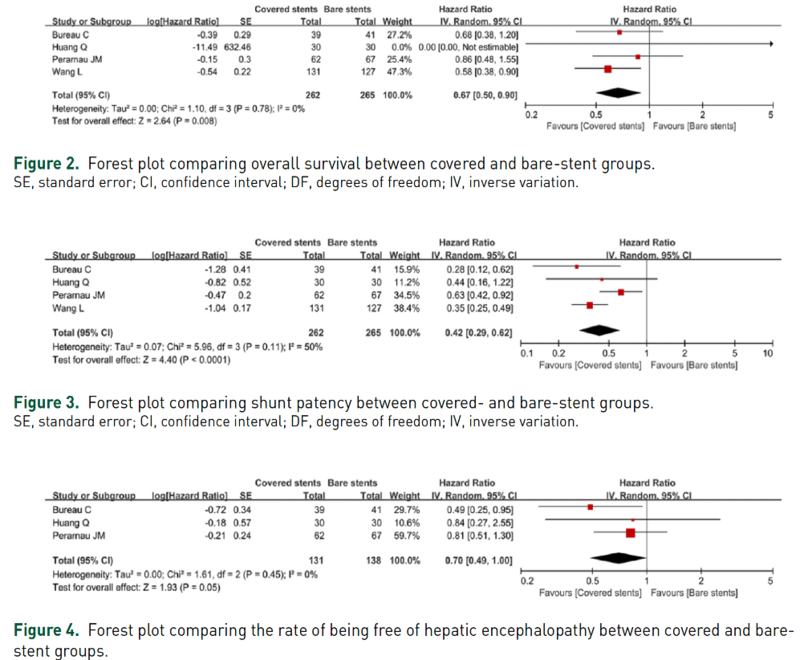
A meta-analysis from 2017 reported that covered stents not only significantly improved the shunt patency, but also significantly decreased the risk of death. Additionally, the risk of hepatic encephalopathy was not increased by using covered stents.
Nonetheless, HE remains a significant complication after TIPS placement even with e-PTFE covered stents.
What is the pathophysiology of post-TIPS HE?
Multiple factors have been proposed to contribute to the development of HE after TIPS placement. First, TIPS results in decreased first pass hepatic clearance of neurotoxins like ammonia but it also increases the splanchnic blood flow that may enhance the delivery of ammonia into the systemic circulation. Also, there is upregulation of intestinal glutaminase activity, which results in increased ammonia production in the intestine. Finally, TIPS placement may lead to parenchymal injury and inadvertent vascular occlusion or compression. These may predispose patients to hepatic ischemia and subsequently HE.
HE has the potential to lead to prolonged duration of hospital admissions, increased number of primary care contacts, impaired quality of life and increased mortality.
What is the incidence of post-TIPS HE?
The median cumulative 1-year incidence of HE after TIPS has been reported to be between 30–50%. Post-TIPS HE still occurs in almost half of patients with e-PTFE covered stents. New onset HE incidence is around 35% and refractory HE occurs in at least 8% of patients. HE has been described within 1 day or as late as 210 days after TIPS. In a cohort including 376 patients, 52% developed post-TIPS HE but only 9% had HE ≥ grade 3. Most cases are mild or moderate and amenable to medical management.
What are the predictors of post-TIPS HE?
Proposed risk factors include advanced age, compromised baseline liver function, history of HE, sarcopenia, presence of excessive shunting and medications.
Age >65, prior history of HE and higher Child-Pugh class are consistent predictors of post-TIPS HE. High MELD score, elevated creatinine, low serum sodium and low albumin values have been associated with post-TIPS HE. High creatinine has been particularly associated with refractory HE.
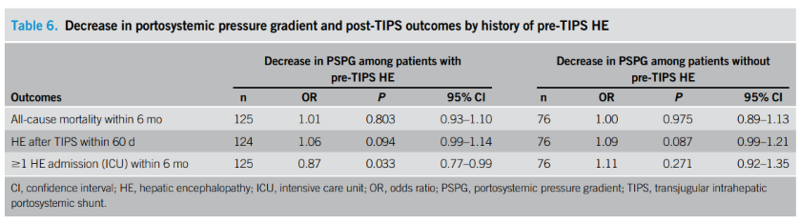
History of HE has been proposed as a relative contraindication for TIPS placement. Nonetheless, a single-center retrospective study reported that HE before TIPS placement for refractory ascites did not predispose patients for increased all-cause mortality, increased risk for experiencing HE without 60 days, or increased risk of hospital admission for HE within 6 months. Patients may be able to undergo TIPS for refractory ascites despite history of HE.
The presence of sarcopenia has been proposed to predispose patients to post-TIPS HE, but Benmassaoud et al published data in 2021 that found no association between sarcopenia with de novo HE or increased mortality. Regarding medications, Dai et al published a cohort study showing that proton pump inhibitors were associated with increased rates of new or worsening post-TIPS HE, however further research is needed. Other medications like opioids, benzodiazepines and diuretics have not been studied in the context of post-TIPS HE.
Portosystemic gradient (PSG) has not been shown to be a reliable predictor of post-TIPS HE. However, persistent spontaneous portosystemic shunt (SPSS) after TIPS placement has been shown to be an independent predictor of complications, including HE.
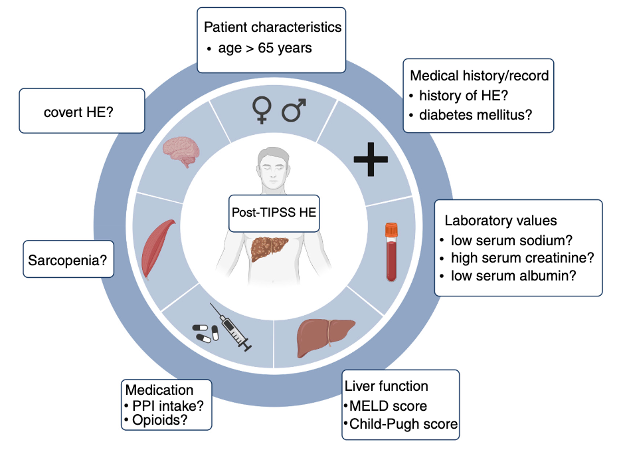
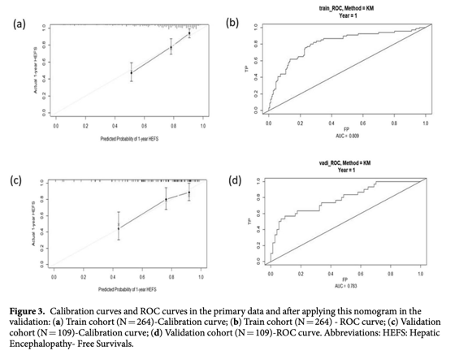
Score systems are being developed with the goal of predicting what patients will develop post-TIPS HE. Yin et al created a nomogram including the variables: age, Child-Turcotte-Pugh class, diabetes mellitus, serum creatinine and serum sodium. Nomogram-derived probabilities of 1-yr hepatic encephalopathy- free survivals after TIPS for esophageal and gastric variceal bleeding were plotted. The C-index of nomograms for prediction of HEFS were 0.772 and 0.773 in the training and validation cohort. The ROC for predicting HEFS was 0.809 and 0.783, respectively.
The need for a validated clinical score system able to predict who will develop post-TIPS HE remains. Also, possible biomarkers are currently lacking.
How can we prevent post-TIPS HE?
Preventive measures include stent size optimization, PSG optimization after TIPS placement, and closure of persistent SPSS after TIPS placement.
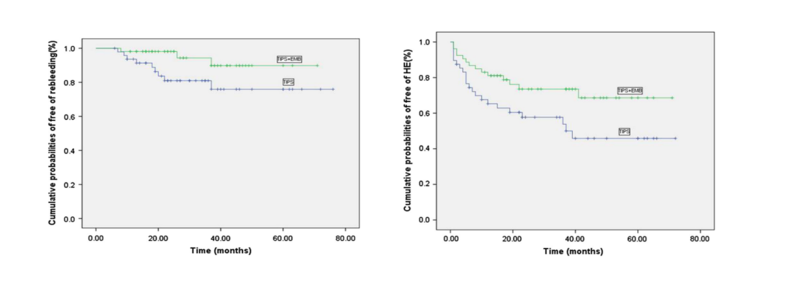
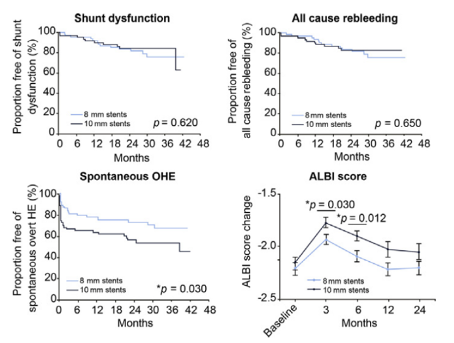
Consistent data has shown that covered stents are superior to bare metal stents. The optimal diameter for TIPS remains uncertain, with prior cohort studies showing no difference between stent diameters. However, a recent randomized controlled trial compared 8 mm and 10 mm stents. As we can see in the graph below, there was no difference between groups regarding shunt patency and risk of rebleeding, but 8 mm stent showed lower spontaneous overt hepatic encephalopathy risk and better liver function reserve.
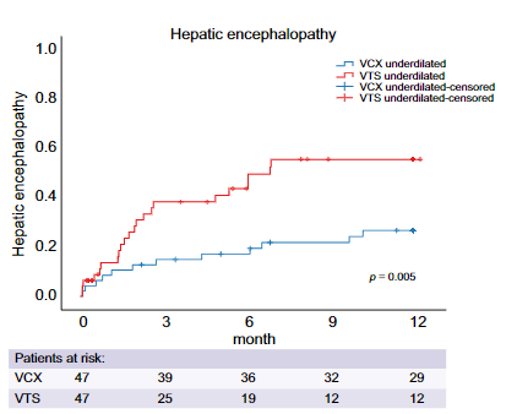
Most devices are e-PTFE covered stents that are dilated to their nominal diameter (8 or 10 mm). One option is to use e-PTFE covered stents dilated to a smaller caliber (under-dilated TIPS) to decrease risk of post-TIPS HE while maintaining symptom control and hemodynamic efficacy. Recent prospective case-control study compared a novel VIATORR Controlled Expansion stent graft (VCX) in under-dilated (8 mm) diameters versus under-dilated (8 mm) VIATORR® TIPS stent grafts (VTS) and found that VCX stent grafts under-dilated to 8 mm do not passively expand to nominal diameter (10 mm) and reduced hospital readmissions due to hepatic encephalopathy (under-dilated VCX n = 11 [23%] versus under-dilated VTS n = 24 (51%), p <0.001), uncontrolled ascites, and heart failure, and improved 1-year survival compared with under-dilated VTS.
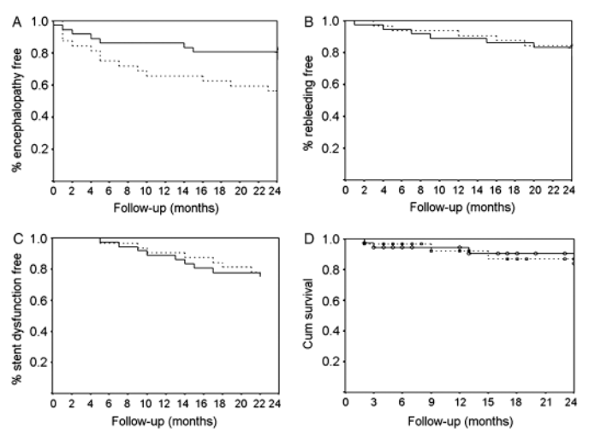
A prospective non-randomized trial compared e-PTFE dilated to 7 and 6 mm versus dilated to 8 mm and found that under-dilated e-PTFE stents were associated with a lower rate of post-TIPS HE and with same clinical efficacy compared with e-PTFE stent dilated to standard diameters. Randomized controlled trials are needed. It has also been proposed that left portal TIPS might prevent post-TIPS HE since the left portal branch supplies a smaller portion of the liver than the right portal branch. A randomized controlled trial demonstrated a significantly lower rate of post-TIPS HE with left versus right TIPS placement without difference in rebleeding, shunt dysfunction and survival.
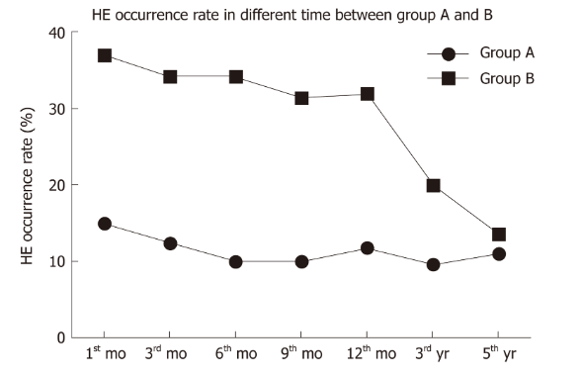
A single-center retrospective study showed a significantly lower post-TIPS HE in patients with left versus right TIPS placement at 1 month (14.94% vs 36.80%; p = 0.028), 3 months (12.48% vs 34.20%; p = 0.025), 6 months (10.03% vs 32.24%; p = 0.010), and 9 months (9.17% vs 31.27%; p = 0.021). There was no significant difference between 1 to 5 years after TIPS placement.
The use of adjunctive variceal embolization may decrease overall shunting and prevent the occurrence of post-TIPS HE. A retrospective study showed that patients who underwent TIPS placement with adjunctive variceal embolization versus TIPS placement alone demonstrated lower post-TIPS HE (p = 0.019) and rebleeding (p = 0.048) without difference in survival (p = 0.466).
Below we provide a summary of all studies on preventive measures for post-TIPS HE including type of stent, stent size optimization, site of stent placement and adjunctive therapy.
Are there nutritional and pharmacologic prophylaxis for post-TIPS HE?
The role of sarcopenia in the development of post-TIPS HE remains unclear. There are currently no specific recommendations for nutritional advice in patients who undergo TIPS placement. However, recommendations tend to be given in accordance with guidelines for secondary HE prevention that include 1.2 to 1.5 g/kg of protein daily intake.
There is no effective pharmacologic primary prevention of HE, therefore no prophylactic therapy is currently recommended. Secondary prevention of HE can be achieved by combination of lactulose with rifaximin. Bass et al, found that rifaximin maintained remission and significantly reduced risk of hospitalization involving HE. Hence, rifaximin was approved for the secondary prevention of overt HE.
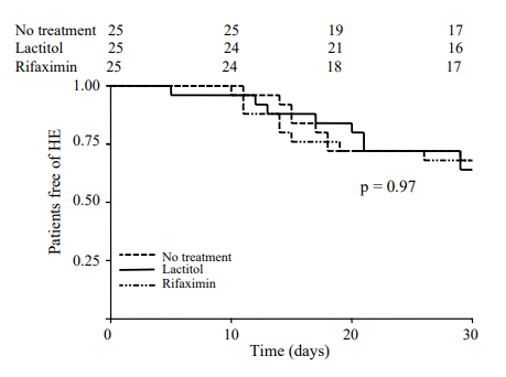
Regarding post-TIPS HE, guidelines currently do not recommend any primary HE prophylaxis after TIPS placement. Riggio et al, reported that rifaximin alone or lactulose alone did not prevent overt post-TIPS HE at least 30 days after TIPS placement.
Nonetheless, a recent randomized controlled trial was performed with 197 patients with alcohol-related cirrhosis who underwent TIPS placement for refractory ascites or secondary prevention of variceal bleeding who were assigned to receive rifaximin (600 mg twice daily) or placebo beginning 14 days before TIPS and continuing for 168 days after procedure. They found that rifaximin reduced the risk of overt post-TIPS HE in patients with alcohol-related cirrhosis with an estimated risk difference of 18 percentage points (CI, -32 to –4 percentage points [P= 0.012]).
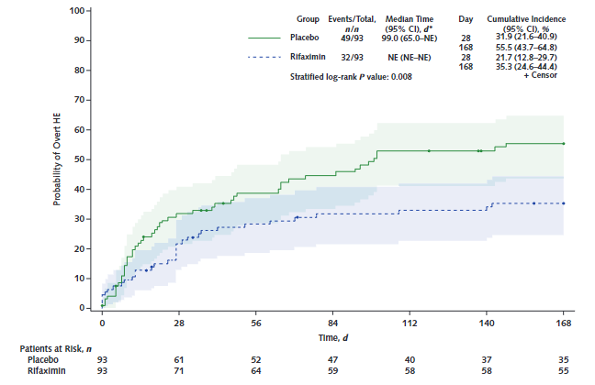
By design, lactulose for HE prevention was not allowed and the medication was stopped in patients that were HE free with this treatment after prior HE episode at the time of enrollment.
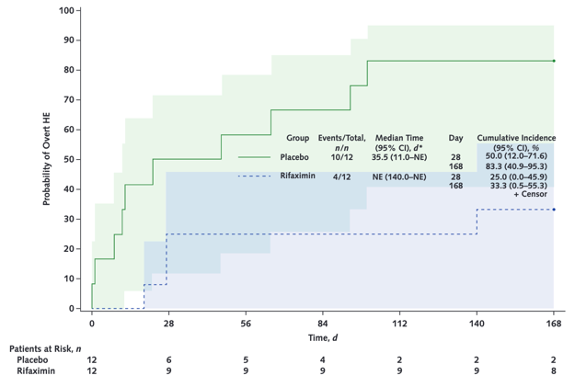
This factor helps explain that in a post hoc analysis of the subset of 24 patients with a previous HE episode, the cumulative incidence of overt HE after TIPS was 33% (CI, 1% to 55%) with rifaximin versus 83% (CI, 41% to 95%) with placebo.
The combination of rifaximin and lactulose has never been tested to prevent post-TIPS HE, but the ongoing PEARL (prevention of post-TIPS hepatic encephalopathy by administration of rifaximin and lactulose) trial will help determine the utility of this combination to prevent post-TIPS HE.
What is the treatment for post-TIPS HE?
The management of post-TIPS HE is similar to the management of HE in patients without TIPS. The mainstays of medical management are lactulose and rifaximin. A randomized controlled trial of lactulose plus rifaximin found that this combination was more effective than lactulose alone in the treatment of overt HE. For more information on why we use lactulose and rifaximin, refer to our prior Why Series post.
Most patients develop mild to moderate HE and medical management is sufficient. For patients with medically refractory HE after TIPS placement, liver transplantation is the definitive treatment. As a bridge to liver transplant or in those who are not transplant candidates, endovascular therapy can be used.
Endovascular therapies include TIPS shunt modification and occlusion. TIPS reduction is an effective intervention for refractory HE. A retrospective study of patients undergoing TIPS reduction (average PSG increased from 8 to 12 mmHg) for refractory HE showed clinical success of 89% with a six-month survival rate of 80%. However, studies have also shown a high rate of recurrence of portal hypertensive complications in consequence this intervention should be reserved for severe refractory cases. Due to the significant risk of iatrogenic complications with shunt occlusions, shunt reduction is a safer and preferred option.
Key Points
- Hepatic encephalopathy remains a frequent and challenging complication from TIPS placement.
- Covered stents with controlled expansion provide the opportunity to precisely adjust the stent diameter and may be an ideal non-pharmacological prophylaxis for post-TIPS HE.
- Research on pharmacological prophylaxis for post-TIPS HE is promising but data from ongoing studies like the PEARL trial are necessary.