Challenges in managing autoimmune hepatitis
Early treatment response
Our patient reported medication compliance, but her AST, ALT and ALP did not improve with four months of corticosteroid and azathioprine therapy. The rapidity of response to treatment, especially improvement in aminotransferase levels within two weeks, has been shown to be an important predictor of longer-term outcomes, including liver-related death and need for transplantation. There are certain factors that predict the response to treatment for autoimmune hepatitis including age, presence of cirrhosis, and ethnicity. A younger age at diagnosis and the presence of cirrhosis are associated with incomplete or absent response to therapy in autoimmune hepatitis.
It is important to note that a proportion of patients (10-15%) are refractory to treatment.
The definitions of treatment response are highlighted in the table below from the AASLD 2019 guidelines on autoimmune hepatitis.
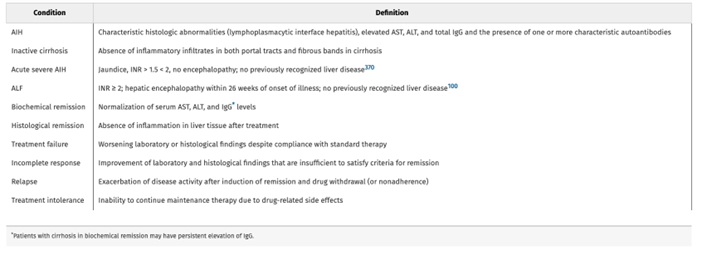
Table 1. Adopted from AASLD guidelines on AIH from 2019
Figures 1 and 2 are examples of algorithms that highlight optimizing therapy before switching to second line therapies.
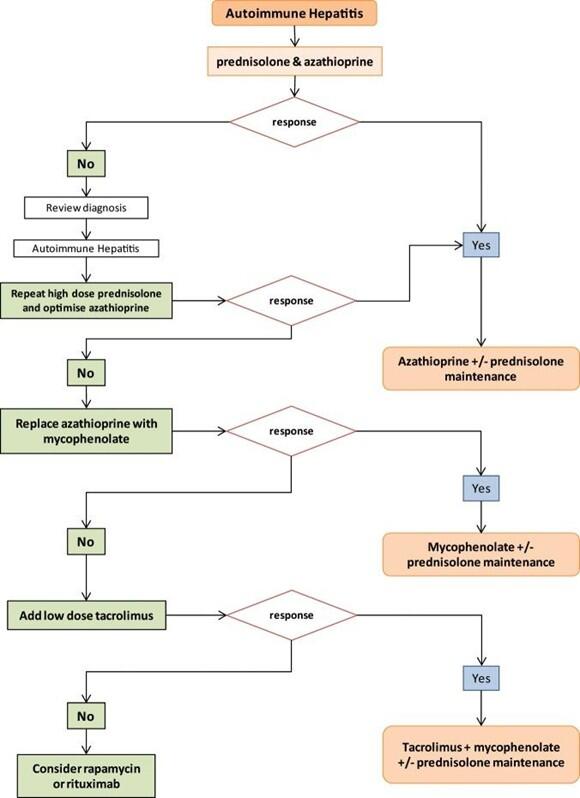
Figure 1. An algorithm on the management of autoimmune hepatitis.
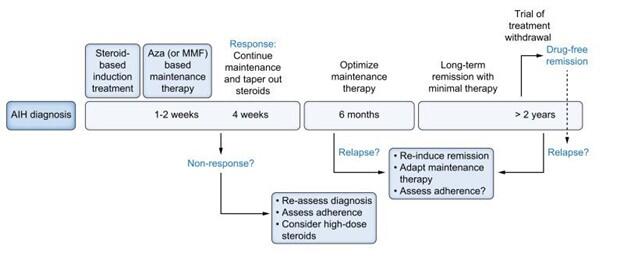
Figure 2. Suggested approach for management of autoimmune hepatitis.
The use of up-front mycophenolate
Emerging data show more patients achieve biochemical remission with mycophenolate mofetil as the first-line therapy as shown in Figure 3. However, because mycophenolate is teratogenic, women of childbearing age must avoid pregnancy during its use and it is recommended to use two forms of contraception.
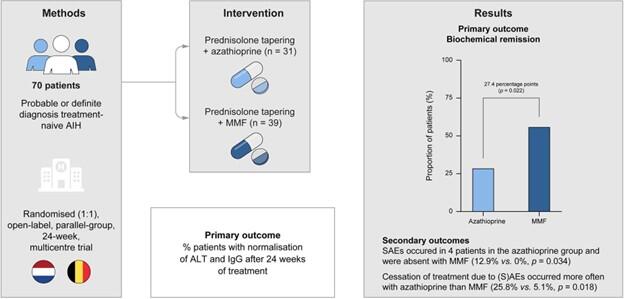
Figure 3. Randomized control trial from Netherlands on a higher rate of biochemical remission at 6 months compared to azathioprine.
The role of repeating liver biopsy
A repeat liver biopsy was obtained to evaluate the response to therapy as the patient exhibited a delayed and atypical response. This showed a significant improvement in the degree of interface hepatitis and an improvement in necroinflammation and lymphocytic infiltration. There continues to be bridging fibrosis and focal regenerative nodule formation (Batts-Ludwig Stage 4/4)
In cases where there is no response to therapy, or when deciding to withdraw therapy, a liver biopsy can be helpful in correlating the regression of fibrosis and determining if an alternative etiology for liver disease is present that could change management.
Conclusions:
- Autoimmune hepatitis is a heterogeneous disease with varying clinical presentations.
- Choosing the right treatment for patients and aiming for biochemical remission early is important.
- Optimizing therapy before switching an agent or calling a treatment failure is crucial.
- In a select group of cases where there remains diagnostic uncertainty and an inadequate treatment response, repeating a liver biopsy can be helpful to guide further management.
